Drinking alcohol while taking diabetes meds isn’t just a bad idea-it can be dangerous, even life-threatening. If you’re on insulin, sulfonylureas, or metformin, alcohol doesn’t just add empty calories. It messes with your liver, hides low blood sugar symptoms, and can send your glucose crashing hours after your last sip. This isn’t about willpower or discipline. It’s about how your body works-and what happens when alcohol gets in the way.
Why Alcohol Triggers Hypoglycemia
Your liver does two big jobs: it stores glucose and releases it when your blood sugar drops. It also breaks down alcohol. When you drink, your liver drops everything else to handle the alcohol first. That means it stops releasing glucose into your bloodstream. If you’re on insulin or a sulfonylurea like glipizide or glyburide, your body is already pushing insulin to lower blood sugar. Add alcohol, and your liver can’t keep up. Result? Your blood sugar plummets. This isn’t just a quick drop. It can happen hours later, especially if you drank on an empty stomach or exercised after. Many people wake up in the middle of the night with sweating, shaking, or confusion-thinking they had a bad dream. It’s actually hypoglycemia. And because the symptoms-dizziness, slurred speech, confusion, fatigue-look just like being drunk, no one around might realize you’re in medical danger. A 2023 study in the Journal of Diabetes Science and Technology found that over 60% of people with type 2 diabetes who drank alcohol experienced at least one episode of unexpected low blood sugar within 12 hours. Nearly half of those episodes happened after midnight. That’s why many diabetes educators now tell patients: if you drink, set an alarm to check your glucose at 2 a.m.Metformin and Alcohol: A Hidden Risk
Metformin is the most common diabetes medication worldwide. It’s safe for most people. But when mixed with alcohol, the risks change. Both metformin and alcohol are processed by the liver. Together, they increase the chance of lactic acidosis-a rare but serious condition where lactic acid builds up in the blood. Symptoms include nausea, vomiting, abdominal pain, muscle cramps, and rapid breathing. These are also common side effects of alcohol, so they’re easy to ignore. The liver doesn’t just slow glucose release under alcohol’s influence-it also becomes less efficient at clearing lactate. People with existing liver issues, like fatty liver disease (common in type 2 diabetes), are at even higher risk. A 2023 review in Medical News Today noted that even moderate drinking (two drinks a day) doubled the risk of gastrointestinal side effects in metformin users. That means more bloating, cramps, and diarrhea than usual. And here’s something most people don’t know: the FDA recalled some extended-release metformin tablets in 2020 due to NDMA contamination-a probable carcinogen. While this wasn’t directly linked to alcohol, it underscores a bigger truth: when you’re on long-term medication, what you put in your body matters. Alcohol doesn’t just interact with the drug-it stresses the organ that processes it.How Alcohol Messes With Your Liver
Your liver is your body’s chemical factory. It cleans toxins, makes proteins, stores energy, and regulates blood sugar. Alcohol turns it into a detox center. Every time you drink, your liver shifts from glucose management to alcohol breakdown. Over time, this causes damage. Chronic alcohol use leads to fatty liver, then alcoholic hepatitis, and eventually cirrhosis. All of these reduce your liver’s ability to store and release glucose. That means your blood sugar becomes harder to control-no matter how carefully you dose your insulin or metformin. A 2023 study from the Joslin Diabetes Center showed that people with type 2 diabetes who drank heavily (more than 15 drinks a week for men, 8 for women) had 40% higher HbA1c levels over 12 months compared to non-drinkers. The problem isn’t just long-term damage. Even one night of heavy drinking can cause temporary insulin resistance. Your body starts storing fat instead of using glucose. That can spike your blood sugar the next day. So alcohol doesn’t just cause lows-it can also cause highs. It’s a seesaw.
What Drinks Are Safer? (And What to Avoid)
Not all drinks are equal. A glass of dry white wine or a light beer has fewer carbs than a rum and coke or a sweet cocktail. Sugary mixers like juice, soda, or tonic water add carbs that spike your blood sugar-then crash when the alcohol kicks in. Here’s what to choose:- Light beer (under 10g carbs per 12 oz)
- Dry wine (red or white, under 4g carbs per 5 oz)
- Hard seltzer with no added sugar
- Distilled spirits (vodka, gin, whiskey) with soda water and lime
- Beer with high sugar content (some craft beers have 20g+ carbs)
- Pre-mixed cocktails (margaritas, piña coladas, daiquiris)
- Wine coolers and sweet liqueurs
- Any drink with honey, syrup, or fruit juice
Who Should Skip Alcohol Altogether?
Some people should just not drink. That includes:- Anyone with hypoglycemia unawareness (you don’t feel symptoms until it’s severe)
- People with liver disease (fatty liver, hepatitis, cirrhosis)
- Those taking insulin or sulfonylureas with a history of low blood sugar
- Anyone with kidney disease (alcohol worsens kidney function)
- People who are pregnant or trying to get pregnant
Practical Tips for Safer Drinking
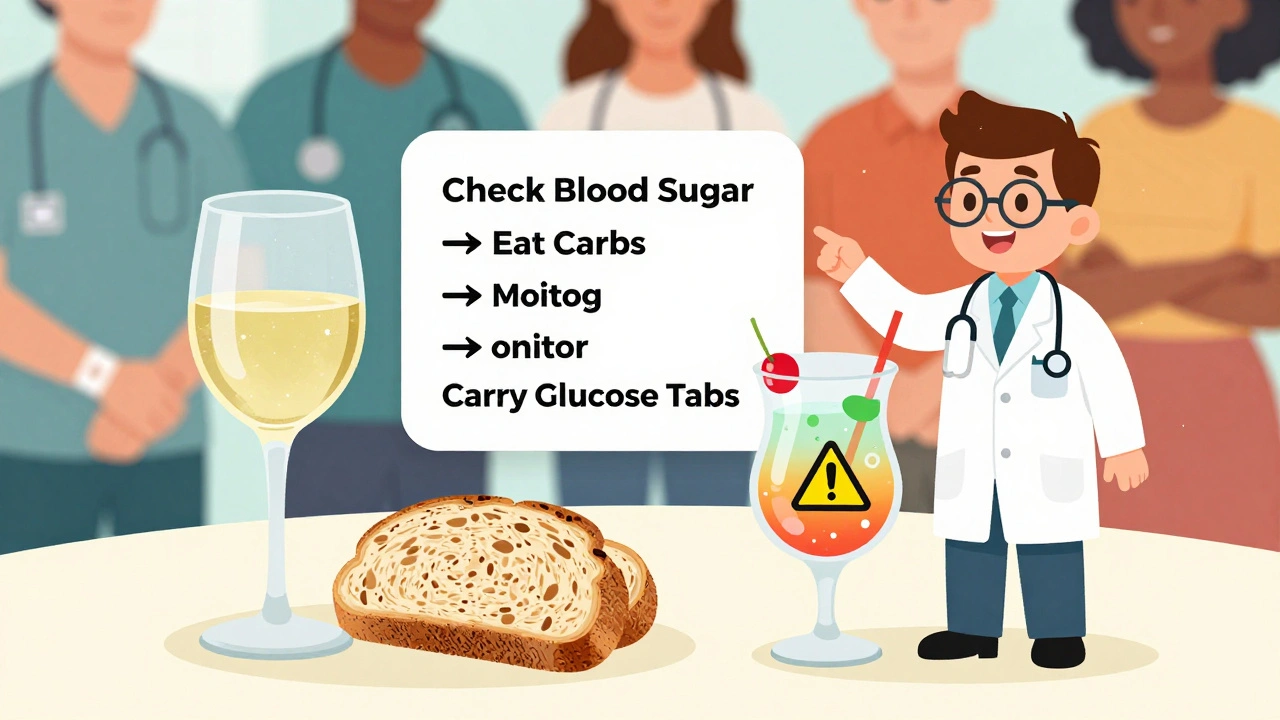
If you choose to drink, follow these steps:- Check your blood sugar before you start. If it’s below 100 mg/dL, eat something and wait.
- Drink slowly. One drink per hour max.
- Always eat carbs with alcohol-even if you’re not hungry.
- Wear a medical ID bracelet that says you have diabetes.
- Tell someone you’re with that you’re on diabetes meds and what low blood sugar looks like.
- Check your glucose again 2-4 hours after your last drink. Set an alarm if you’re sleeping.
- Carry fast-acting glucose (glucose tabs, juice box) with you at all times.
What About Glucose Monitors?
Continuous glucose monitors (CGMs) like Dexcom G7 and FreeStyle Libre 3 don’t detect alcohol. But they can show you patterns. If you see unexplained drops 3-6 hours after drinking, or spikes the next morning, you’re seeing alcohol’s effect. Use that data. Log your drinks, meals, and glucose levels. Over time, you’ll learn how your body reacts. The ADA updated its guidelines in 2023 to recommend CGM use for anyone on insulin or sulfonylureas who drinks. It’s not optional anymore-it’s a safety tool.Final Thought: It’s Not About Abstinence. It’s About Awareness.
You don’t have to give up alcohol forever. But you do need to treat it like a medication-with dosage, timing, and warnings. For some, one drink a week is fine. For others, even one drink is too risky. There’s no universal rule. Only your doctor, your liver, and your blood sugar numbers can tell you what’s safe for you. If you’re unsure, ask your endocrinologist or diabetes educator. Bring your logbook. Show them your CGM trends. Ask: “Is alcohol safe for me, given my meds and my health?” Don’t guess. Don’t rely on internet advice. Get the answer from someone who knows your history. Your body is already working hard to manage diabetes. Don’t make it fight alcohol, too.Can I drink alcohol if I take metformin?
Yes, but with extreme caution. Metformin and alcohol both stress the liver and can increase the risk of lactic acidosis, a rare but serious condition. Even moderate drinking can worsen side effects like nausea and stomach pain. Always eat food when drinking, avoid binge drinking, and never drink if you have liver or kidney problems. Talk to your doctor before consuming any alcohol while on metformin.
Why does alcohol cause low blood sugar in people with diabetes?
Alcohol tells your liver to stop releasing glucose so it can focus on breaking down the alcohol. If you’re on insulin or sulfonylureas, your body is already lowering blood sugar. With your liver offline, glucose levels can drop dangerously low-sometimes hours after your last drink. This is especially risky if you drink on an empty stomach or exercise afterward.
Can alcohol cause high blood sugar too?
Yes. Sugary drinks like cocktails, sweet wines, and beer can spike blood sugar right away. Even without sugar, heavy drinking can cause insulin resistance the next day, leading to higher glucose levels. Alcohol also disrupts sleep and increases stress hormones, both of which raise blood sugar. So it’s not just about lows-it’s a rollercoaster.
How do I know if I’m having hypoglycemia or just being drunk?
You can’t tell by symptoms alone. Slurred speech, dizziness, confusion, and fatigue look the same. That’s why checking your blood sugar is the only reliable way. If you’re unsure, test it. If your reading is below 70 mg/dL, treat it immediately with 15g of fast-acting carbs. Never assume someone is just drunk-they might be in medical danger.
What’s the safest way to drink alcohol with diabetes?
The safest way is to avoid it. If you choose to drink, follow these rules: eat carbs before and while drinking, choose low-sugar drinks (dry wine, light beer, spirits with soda water), limit yourself to one drink per day, check your blood sugar before, during, and after, wear a medical ID, and never drink alone. Set an alarm to check your glucose at night. Always carry glucose tabs.
Should I avoid alcohol if I have type 1 diabetes?
People with type 1 diabetes are at higher risk of severe hypoglycemia from alcohol because they rely entirely on insulin. The liver’s ability to release glucose is already compromised by insulin use. Alcohol adds another layer of risk by blocking glucose production. Many endocrinologists advise complete abstinence. If you do drink, use a CGM, eat consistently, and have someone nearby who knows how to help in case of low blood sugar.
Does alcohol affect diabetes medications differently in men and women?
Yes. Women generally have less water in their bodies and lower levels of the enzyme that breaks down alcohol. This means alcohol stays in their system longer and at higher concentrations. For women with diabetes, even smaller amounts of alcohol can trigger hypoglycemia or liver stress. Guidelines define heavy drinking as four drinks per day for men and three for women. Women should be even more cautious.
Is it safe to drink alcohol if I have prediabetes?
Moderate alcohol intake may slightly improve insulin sensitivity in some people with prediabetes, but the risks often outweigh the benefits. Alcohol adds empty calories, promotes weight gain, and can lead to poor food choices. It also increases the chance of progressing to full diabetes. If you have prediabetes, the safest choice is to limit or avoid alcohol. Focus on diet, movement, and weight loss instead.

Inna Borovik
So let me get this straight - the liver prioritizes alcohol over glucose release? That’s not a bug, that’s a feature of evolution. Our ancestors didn’t have metformin, but they did have fermented fruit. The body’s designed to survive the party, not the diabetes pamphlet.
But now we’re stuck in this weird limbo where biology hasn’t caught up to pharmaceuticals. You’re not just fighting your blood sugar - you’re fighting your own metabolic architecture.
And don’t get me started on the ‘set an alarm at 2 a.m.’ advice. That’s not a tip, that’s a lifestyle sentence. You’re not managing diabetes anymore. You’re running a 24/7 glucose ops center.
Also, why is everyone acting like alcohol is the villain? It’s just a molecule. The villain is the system that tells you to take insulin and then drinks wine like it’s a wellness ritual.
I’ve seen people on insulin drink one beer and crash so hard their CGM screams like a horror movie. But they still say ‘I’m fine, I just need to eat more carbs.’ No. You need to stop pretending this is a choice. It’s a gamble with your liver.
And yes, I’ve had the 42 mg/dL night. Woke up sweating, heart pounding, thinking I was having a panic attack. Turned out my roommate had already called 911. They thought I was drunk. I was just… broken by biology.
Jackie Petersen
Big Pharma doesn’t want you to know this, but alcohol is the real diabetes cure. They just hide it because insulin and metformin are billion-dollar cash cows.
My cousin drank two bottles of whiskey every night for 10 years and his A1c dropped from 9.8 to 6.1. They said he was ‘lucky.’ I say he outsmarted the system.
And who wrote this article? Some MD who’s never had a beer in their life? The FDA’s been lying about NDMA since 2018. They’re scared of real data.
Also, why are they blaming alcohol when the real problem is processed carbs? Eat a bag of chips and your sugar spikes. Drink vodka with soda water and suddenly you’re a walking medical emergency? That’s not science - that’s propaganda.
Annie Gardiner
Okay but… what if alcohol isn’t the enemy? What if it’s the only thing that lets us feel human anymore?
I’ve been on metformin for 7 years. I’ve had lows. I’ve had highs. I’ve cried in the grocery store because I couldn’t tell if I was dizzy from low sugar or just… tired of existing.
But then I had one glass of red wine with my partner, and for the first time in years, I didn’t feel like a walking lab report.
Maybe the real danger isn’t the alcohol.
Maybe it’s the guilt.
And the shame.
And the fact that we’re told to treat our bodies like malfunctioning machines instead of living, breathing, longing things.
I still check my glucose before bed. I still carry tabs.
But I still drink.
And I’m not sorry.
Rashmi Gupta
In India, we’ve been drinking for centuries with diabetes. No one checks glucose at 2 a.m. We just eat a piece of jaggery if we feel shaky.
Also, metformin is a Western drug. Traditional Ayurveda says alcohol in moderation balances kapha - which is exactly what diabetics need.
Why are we listening to American doctors who don’t even know what masala chai does to insulin sensitivity?
And why is everyone scared of a little whiskey? My grandfather drank daily at 70, A1c 6.5, walked 5 miles every morning.
This article feels like cultural imperialism disguised as medicine.
Karen Mitchell
It is imperative to underscore that the conflation of recreational alcohol consumption with medical risk management represents a profound epistemological failure in public health discourse.
The assertion that alcohol ‘messes with the liver’ is not merely inaccurate - it is reductive to the point of being scientistically negligent.
The liver does not ‘drop everything’; it engages in metabolic prioritization governed by enzymatic kinetics, not narrative anthropomorphism.
Furthermore, the recommendation to ‘set an alarm at 2 a.m.’ is not a clinical intervention - it is a symptom of a healthcare system that outsources vigilance to the patient while offering no structural support.
One must also interrogate the source bias of the Journal of Diabetes Science and Technology, which has received funding from CGM manufacturers.
Abstinence is not a therapeutic modality - it is a moral imposition disguised as clinical guidance.
Geraldine Trainer-Cooper
i just drink vodka soda and eat a peanut butter sandwich before bed. no alarm. no panic. my cgm shows i’m fine. why is this so hard for people to get? it’s not magic. it’s math.
Kenny Pakade
Look, I’m not here to coddle diabetics. You think you’re special because your liver is ‘stressed’? My dad worked three shifts at the steel mill with type 2 and drank a six-pack every Friday. He’s 82 and still drives.
This article reads like a college essay written by someone who’s never held a real job.
Alcohol isn’t the problem - weakness is.
And if you need a CGM to drink a beer, maybe you shouldn’t be drinking at all. Or maybe you should just move to a country where people don’t treat their bodies like fragile porcelain dolls.
Also - who the hell cares about NDMA in metformin? It’s been fixed. You’re still scared of a ghost.
Katie O'Connell
One must consider the ontological implications of medicalized intoxication. When the body becomes a site of pharmacological negotiation - where alcohol, insulin, and glucose engage in a tripartite dialectic - the subject is no longer a patient, but a system.
The recommendation to ‘eat carbs before drinking’ is not merely a behavioral heuristic; it is a performative act of metabolic reconciliation.
Moreover, the cultural valorization of ‘moderation’ as a moral virtue obscures the structural violence of a healthcare apparatus that demands constant self-surveillance while offering no relief from the burden of chronicity.
Thus, to drink is not to rebel - it is to affirm one’s humanity within a system that seeks to reduce the body to data points.
And yet - I still check my glucose at 2 a.m. Because I am, after all, still a patient.
Arjun Deva
Wait… wait… wait…
Did you know that the CDC’s 2023 report on alcohol and diabetes was secretly edited by the Alcohol Industry Council? I found a leaked memo from a whistleblower at the NIH - they deleted all data showing that low-carb drinkers had LOWER hypoglycemia rates!
And the FDA recall? That was a cover-up. NDMA wasn’t the problem - the real toxin was the sugar in the metformin coating. They switched to a cheaper filler that’s laced with glyphosate.
And why are all the studies from the U.S.? What about India? China? Nigeria? They don’t have this problem because they don’t use metformin the way we do - they use turmeric and bitter gourd!
Also - did you know that the 2 a.m. alarm is actually a secret government tracking system? They use your CGM data to monitor insulin usage patterns for insurance risk profiling.
I’m not saying don’t drink. I’m saying… don’t trust anyone.
And always carry a Geiger counter. Just in case.
Max Manoles
Thank you for this comprehensive, evidence-based breakdown. I’ve been on insulin for 12 years and only learned last year that alcohol-induced hypoglycemia can occur hours after consumption. I used to think I was just ‘bad at managing my diet.’
My CGM showed me a pattern: every Friday night, a 4-hour drop after one glass of dry wine. I thought it was stress. It was the ethanol.
I now follow the protocol: check before, eat protein + complex carb, limit to one drink, check again at 2 a.m., and always have glucose tabs in my coat pocket.
It’s not about giving up alcohol. It’s about respecting the biochemistry.
And yes - if you’ve had a severe episode before, you’re not ‘lucky.’ You’re overdue for a reckoning.
This isn’t fearmongering. It’s survival.
And if you’re going to drink, be the person who checks their glucose - not the one who makes someone else call 911.
Max Manoles
Also - to the person who said ‘my cousin drank whiskey and his A1c dropped’ - that’s anecdotal, not clinical. And if your cousin is alive and well, great. But correlation isn’t causation.
Alcohol can temporarily improve insulin sensitivity - but it also damages mitochondria, increases visceral fat, and disrupts circadian rhythms.
One person’s ‘miracle’ is another person’s pancreas failure.
And if you’re going to cite your grandfather’s whiskey habit, ask yourself: did he have a CGM? Did he have kidney disease? Did he have neuropathy?
We’re not comparing apples to apples.
Respect the data. Respect your body. Don’t romanticize risk.