When you stand up from a chair, your body should automatically adjust your blood pressure to keep you from feeling dizzy or fainting. But for people with autonomic neuropathy, that automatic response breaks down. The result? Sudden drops in blood pressure, lightheadedness, blackouts, and a host of gastrointestinal problems that make eating, digesting, and even leaving the house feel like a daily battle.
What Exactly Is Autonomic Neuropathy?
Autonomic neuropathy isn’t just one symptom-it’s a breakdown in the nerves that control your body’s silent functions: heartbeat, digestion, blood pressure, sweating, and bladder control. These nerves don’t respond to your will. They work behind the scenes, like an invisible autopilot. When they’re damaged, your body loses its ability to regulate itself properly.
Most cases-85 to 90%-are linked to long-term diabetes. High blood sugar slowly damages the tiny blood vessels that feed these nerves. Over time, the nerves starve and misfire. But it’s not just diabetes. Autoimmune disorders, certain chemotherapy drugs like vincristine, Parkinson’s disease, and even some viral infections can trigger it too. The problem? Many people don’t realize they have it until symptoms become severe. Studies show doctors miss the diagnosis in 70% of cases, often mistaking dizziness or nausea for something else.
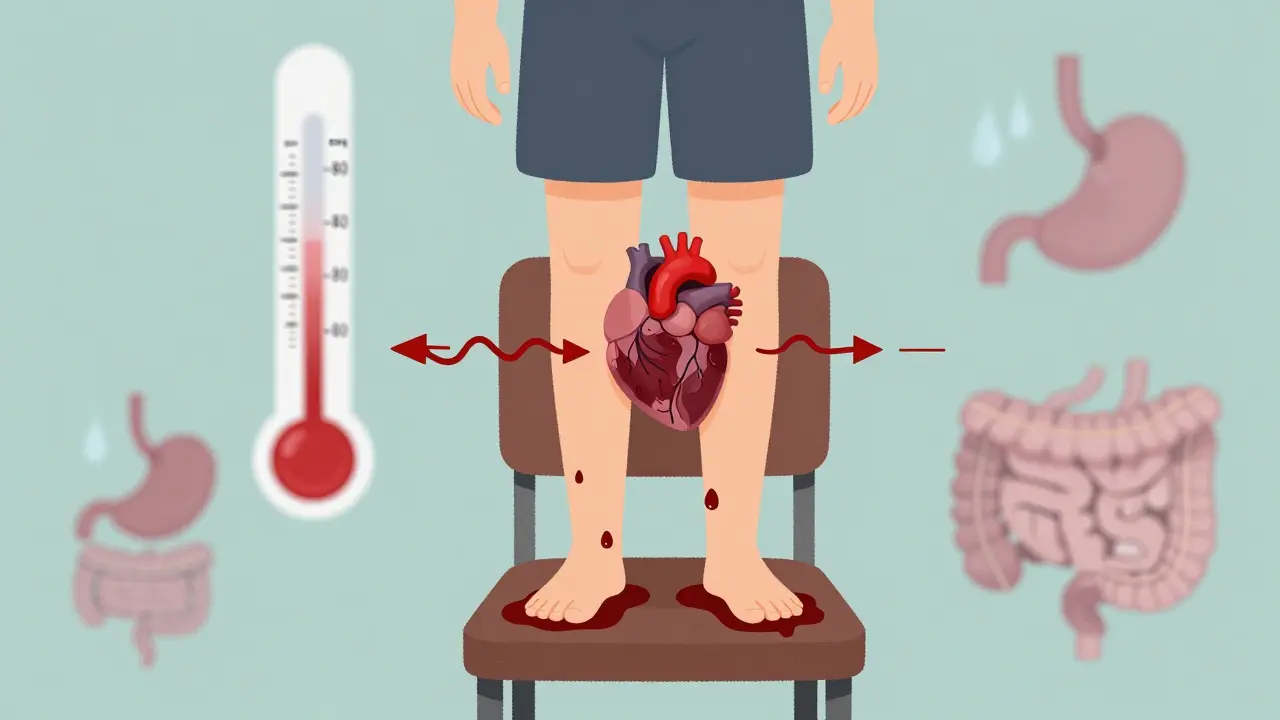
Why Your Blood Pressure Crashes When You Stand Up
Standing up should trigger your body to squeeze blood vessels and speed up your heart just enough to keep blood flowing to your brain. In autonomic neuropathy, that signal never gets through. The sympathetic nerves that handle this reflex are damaged. So when you stand, gravity pulls blood down into your legs-and your body doesn’t fight back.
This is called orthostatic hypotension. It’s defined as a drop in systolic blood pressure of at least 20 mmHg-or diastolic by 10 mmHg-within three minutes of standing. In severe cases, systolic pressure can plummet from 120 to 85 mmHg in under 30 seconds. That’s not just dizziness. That’s passing out, falling, and breaking bones.
Up to 30% of people with diabetic autonomic neuropathy experience this. But it’s not always that obvious. Some people feel a foggy head, blurred vision, or nausea instead of a full blackout. In a 2021 study of 450 patients, 68% had blood pressure readings below 90 mmHg systolic during standing tests. Over 40% had symptoms at least once a week.
Then there’s POTS-Postural Orthostatic Tachycardia Syndrome. It’s not the same as orthostatic hypotension. In POTS, your blood pressure doesn’t drop much, but your heart races-often over 120 beats per minute-just from standing. It’s more common in young women and affects 1 to 3 million Americans. Many people with POTS also have autonomic neuropathy. The line between them is blurry, and doctors still debate whether they’re the same condition or different sides of the same coin.
What Happens in Your Gut When Nerves Go Wrong
While blood pressure issues grab attention, the gastrointestinal symptoms are just as disabling-and often more embarrassing. About one in three people with autonomic neuropathy develop gastroparesis: a condition where the stomach empties too slowly. Food sits there for hours, fermenting, bloating, and vomiting.
Scintigraphy tests show that 30% of diabetic patients with autonomic neuropathy have delayed gastric emptying. That means after eating, more than 10% of food is still in the stomach four hours later. In severe cases, it’s over 30%. Patients report vomiting up meals hours after eating, especially at night. One Mayo Clinic study found 78% of these patients vomited at night, and 45% did so every day.
Constipation is just as common. Bowel movements drop from the normal 4-5 times a week to just 1 or 2. Some people go days without pooping. Others alternate between constipation and sudden, watery diarrhea-often at night. This isn’t just inconvenient. It’s exhausting. And it’s not caused by diet. It’s nerve damage.
Behind the scenes, something else is happening: small intestinal bacterial overgrowth, or SIBO. When the gut doesn’t move food along properly, bacteria that belong in the colon creep into the small intestine. They feast on undigested carbs, producing gas, bloating, and diarrhea. Studies show 52% of autonomic neuropathy patients with GI symptoms have SIBO-compared to only 15% in healthy people.
Swallowing can also become a problem. The esophagus loses its ability to push food down. About 40-60% of patients show abnormal muscle contractions on manometry tests. That leads to choking, chest pain, and the feeling that food is stuck.

How Doctors Diagnose It
There’s no single blood test for autonomic neuropathy. Diagnosis relies on a mix of symptom reports and objective tests.
The 10-minute active stand test is the first step. You lie down for five minutes, then stand up while your blood pressure and heart rate are monitored. A drop of 20 mmHg systolic or 10 mmHg diastolic confirms orthostatic hypotension. If your heart races over 30 bpm without a pressure drop, it’s likely POTS.
Heart rate variability testing during deep breathing is another key tool. Healthy people’s heart rates naturally rise when inhaling and fall when exhaling. In autonomic neuropathy, that variation shrinks. A ratio of expiration to inspiration under 1.1 is abnormal.
For GI issues, gastric emptying scintigraphy is still the gold standard. You eat a meal with a harmless radioactive tracer, then get scanned over four hours. If more than 10% of the meal is still in your stomach, you have gastroparesis. A newer option is the wireless motility capsule-a pill you swallow that tracks pressure, pH, and temperature as it moves through your gut. It’s 92% accurate compared to scintigraphy.
Doctors also use questionnaires like the COMPASS-31, which scores symptoms from 0 to 100. A score above 30 means significant autonomic dysfunction. It’s not perfect, but it’s reliable-85% of the time, it matches up with lab test results.
Treatment: What Actually Works
There’s no cure for autonomic neuropathy. But there are ways to manage symptoms-and many people find real relief.
For blood pressure drops, fludrocortisone is often the first choice. It helps your body hold onto salt and water, increasing blood volume. About 60% of people see improvement. But it can cause high blood pressure when lying down-a dangerous side effect. Midodrine is another option. It tightens blood vessels, helping to keep pressure up when standing. It works for 70% of users, but you have to take it at the right times-no doses after 6 PM or you’ll sleep with high blood pressure.
For POTS, ivabradine is a game-changer. It slows the heart without lowering blood pressure. In one study, 65% of patients saw their heart rate drop by 15-25 beats per minute. That means less dizziness, fewer fainting spells, and more energy.
For the gut, things are trickier. Metoclopramide used to be standard-it speeds up stomach emptying. But it carries a black box warning: long-term use can cause irreversible twitching movements called tardive dyskinesia. Erythromycin works well short-term, but the body gets used to it in weeks. That’s why many doctors now turn to pyridostigmine. It’s not a powerhouse, but it improves symptoms in 55% of patients with fewer side effects.
Non-drug approaches are just as important. Wearing compression stockings (30-40 mmHg) reduces orthostatic symptoms by 35%. Abdominal compression garments help with bloating and nausea. Eating six small meals a day instead of three big ones cuts vomiting episodes by half. Cutting fat to under 25 grams and fiber to under 10 grams a day helps food move through the stomach faster.
And don’t underestimate salt. Many patients report that adding salt to meals helps keep their blood pressure up. One Reddit user wrote, “I went from passing out twice a day to walking around for four hours straight after upping my salt intake.”

What Life Is Really Like
Behind the medical terms are real people. On Reddit’s r/dysautonomia, 82% of over 1,200 respondents said orthostatic symptoms were their biggest struggle. Many describe “brain fog” during low-pressure episodes-like their thoughts are underwater. Over 70% wear compression gear daily. Nearly 90% avoid hot showers, saunas, and humid weather because heat makes blood pressure drop worse.
For GI symptoms, social life falls apart. Sixty-two percent say dietary restrictions have ruined dinners out. Fifty-five percent avoid restaurants entirely because they can’t predict when they’ll vomit or need to rush to the bathroom.
One user on HealthUnlocked wrote: “The low-fat, low-residue diet cut my vomiting from five times a day to once every three days. It’s not fun. But it’s worth losing pizza night.”
Diagnosis takes years. On average, people see three doctors before getting the right answer. The delay? Nearly five years. That’s five years of being told it’s anxiety, depression, or “just aging.”
The Future: What’s Coming
Things are changing. The American Diabetes Association now recommends annual autonomic screening for anyone with diabetes longer than seven years. That could uncover half a million new cases yearly.
New biomarkers are emerging. Blood tests measuring neurofilament light chain-a protein released when nerves are damaged-can now predict severity with 78% accuracy. That means doctors might detect autonomic neuropathy before symptoms even start.
Fecal microbiota transplants are being tested for SIBO-related GI symptoms. Early results show 40% improvement in quality of life after six months.
And the diagnostic bar is lowering. The 2025 American College of Cardiology guidelines will redefine orthostatic hypotension as a drop of just 15 mmHg systolic-not 20. That means earlier detection, earlier help.
But the reality remains: severe autonomic neuropathy still cuts life expectancy by over eight years compared to diabetics without nerve damage. The stakes are high. And awareness is still too low.
Can autonomic neuropathy be reversed?
In most cases, no. Once nerves are damaged, they don’t fully heal. But if the cause is caught early-like uncontrolled diabetes-the damage can be slowed or stopped. Tight blood sugar control, quitting smoking, and managing blood pressure can prevent further harm. Some people even see partial improvement in symptoms over time with aggressive management.
Is autonomic neuropathy the same as POTS?
Not exactly. POTS is a specific type of autonomic dysfunction where your heart races when you stand, but your blood pressure doesn’t drop much. Autonomic neuropathy is the broader umbrella term for nerve damage affecting involuntary functions. Many people with autonomic neuropathy have POTS, but not everyone with POTS has nerve damage. Some experts see POTS as part of the autonomic neuropathy spectrum; others treat it as a separate condition. The distinction matters because treatment can differ.
What foods should I avoid with gastroparesis?
Avoid high-fat foods (fried items, cream sauces), high-fiber foods (raw vegetables, whole grains, beans), carbonated drinks, and alcohol. These slow gastric emptying even more. Stick to cooked vegetables, lean meats, low-fiber breads, and liquids like broths and smoothies. Eating small, frequent meals is more important than any single food restriction.
Why do I feel dizzy even when I’m sitting down?
Autonomic neuropathy can cause blood pressure to drop even without standing. Heat, large meals, alcohol, or dehydration can trigger it. Your body can’t adjust fast enough. If you’re dizzy while sitting, check your blood pressure. You might be experiencing a sudden drop from internal triggers-not just posture. This is common in advanced cases.
Can I still exercise with autonomic neuropathy?
Yes-but differently. Avoid standing exercises if you get dizzy. Try seated cycling, swimming, or upper-body workouts. Keep hydration and salt intake high. Warm up slowly. Avoid hot environments. Some people use compression gear during activity. Even light movement helps circulation and prevents muscle wasting. Always monitor your symptoms. If you feel faint, stop immediately.
Steven Lavoie
This is one of the most comprehensive breakdowns of autonomic neuropathy I’ve ever seen. The way you connected POTS, gastroparesis, and SIBO under the same autonomic umbrella is clinically spot-on. Most people think it’s just ‘low blood pressure’-but this? This is systemic failure of the body’s silent autopilot. I’ve seen patients with 5-year diagnostic delays, mislabeled as anxiety or depression. It’s criminal how underdiagnosed this is.
Sachin Bhorde
bro i had this for years n no doc would believe me. they said i was ‘just tired’ or ‘depressed.’ then i got a motility capsule test-turns out my stomach was holding food for 6+ hours. pyridostigmine saved my life. also salt. so much salt. now i wear compression socks like they’re leggings. no shame. also avoid hot showers like the plague. heat = instant faint.
Salome Perez
Thank you for writing this with such clarity and compassion. As a nurse who works in endocrinology, I see this daily-patients who’ve been gaslit by the medical system for years. The COMPASS-31 score is underutilized, and I’m thrilled to see the 2025 guidelines lowering the diagnostic threshold. Early detection saves lives. Also, the fecal transplant trials for SIBO? Groundbreaking. I’ve had patients go from bedridden to hiking again after one course. Hope is real here.
Raven C
While I appreciate the clinical depth, I must point out that the reliance on ‘Reddit anecdotes’ as evidence is... problematic. The assertion that ‘salt helped’ is not a controlled variable-it’s anecdotal confirmation bias. And the suggestion that dietary fat restriction alone improves gastroparesis? That’s dangerously reductive. The autonomic nervous system is not managed by a keto diet or a salt shaker. This post, while well-intentioned, risks promoting pseudoscientific self-management over evidence-based care.
Josh Potter
Y’ALL. I just got diagnosed last month. I was throwing up after every meal. Now I eat 6 tiny meals, wear my compression leggings like a second skin, and drink broth like it’s water. I’m not fixed-but I’m not dying anymore. Also, ivabradine? It’s like someone turned down the volume on my heart. I can now walk to the mailbox without feeling like I’m gonna pass out. Thank you for this. I finally feel seen.
Victoria Rogers
Why is this even a thing? I mean, if you’re diabetic, you should’ve just controlled your sugar. No one’s forcing you to eat donuts. And now we’re giving out fancy pills and capsules and compression gear? This is just another way the medical-industrial complex profits off people who won’t take responsibility. Maybe if you didn’t eat carbs, you wouldn’t need a motility capsule.
Jody Patrick
Diabetes causes this. Stop blaming the system. Control your blood sugar.
Steven Lavoie
That’s not how this works, Jody. Autonomic neuropathy isn’t a moral failure. It’s a biochemical cascade-sometimes triggered by diabetes, sometimes by chemo, sometimes by a virus nobody even knew existed. You don’t ‘choose’ to have your nerves die. And telling people to ‘just control sugar’ ignores the fact that 15% of cases aren’t diabetes-related at all. This isn’t about willpower. It’s about biology.
Martin Spedding
They say it’s from diabetes… but what if it’s from 5G? Or the vaccines? Or the water? I’ve got a cousin who got this after his second shot. He’s on a 7-day salt fast now. No meds. Just lemon water and willpower. Also, why do all the studies say ‘diabetes’? Coincidence? I think not.
Jonathan Morris
They’re hiding the real cause. The FDA approved fludrocortisone in 1954. That’s the same year the first synthetic sweetener hit the market. Coincidence? The pharmaceutical industry doesn’t want you to know that salt and compression stockings work better than their $300/month drugs. They profit from chronic disease. This post? It’s a Trojan horse for Big Pharma.