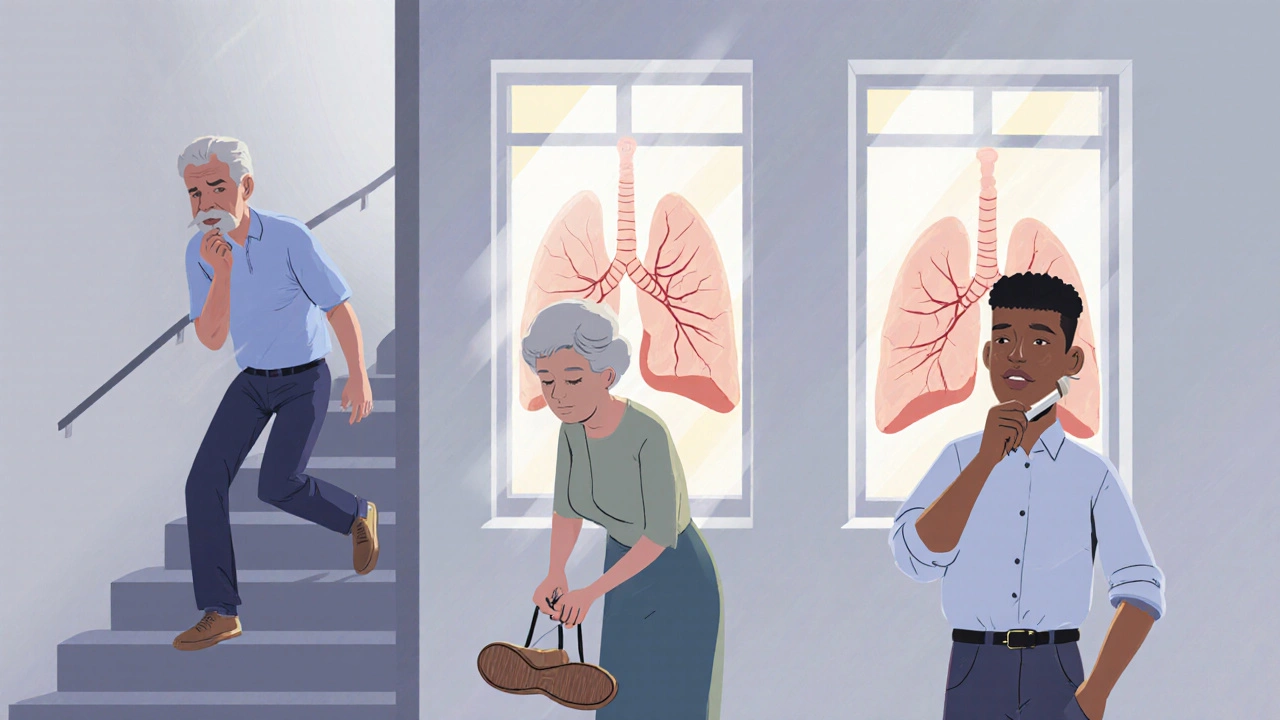
Chronic Obstructive Pulmonary Disease, or COPD, isn’t just a cough that won’t go away. It’s a progressive lung condition that slowly steals your ability to breathe - and most people don’t realize they have it until it’s already advanced. If you’ve been told you’re ‘just out of shape’ or ‘getting older,’ but you’re constantly winded climbing stairs or tying your shoes, it might be more than that. COPD affects 380 million people worldwide, and in many cases, it’s been silently worsening for years before diagnosis.
What Exactly Is COPD?
COPD isn’t one disease - it’s a group of lung conditions that block airflow and make breathing harder. The two main types are chronic bronchitis, where the airways are inflamed and produce too much mucus, and emphysema, where the air sacs in the lungs are damaged and can’t hold air properly. Most cases - 85 to 90% - are caused by smoking. But long-term exposure to air pollution, chemical fumes, or secondhand smoke can also trigger it.
There’s no cure. Once lung tissue is damaged, it doesn’t heal. But that doesn’t mean you’re out of options. The goal isn’t to reverse the damage - it’s to slow it down, manage symptoms, and keep you moving as long as possible.
The Four Stages of COPD: What Your Lung Function Tells You
COPD is staged using a simple breathing test called spirometry. It measures how much air you can forcefully blow out in one second - that’s your FEV1. The result is compared to what’s normal for someone your age, height, and gender. The lower your FEV1 percentage, the worse your lung function.
- Stage 1 (Mild): FEV1 is 80% or higher. You might have a persistent cough and some mucus, especially in the morning. Many people ignore these signs, thinking it’s just a smoker’s cough or they’re not fit enough. But even at this stage, lung damage is happening.
- Stage 2 (Moderate): FEV1 drops to 50-79%. Now, shortness of breath kicks in during everyday activities - walking to the mailbox, doing light housework, or climbing a flight of stairs. You start stopping to catch your breath more often. This is the stage where most people finally see a doctor.
- Stage 3 (Severe): FEV1 falls to 30-49%. Breathing becomes a constant effort. Simple tasks like getting dressed or making a meal leave you gasping. Flare-ups - called exacerbations - happen more frequently, often requiring antibiotics or steroids. Hospital visits become more common.
- Stage 4 (Very Severe): FEV1 is below 30%, or below 50% with chronic low oxygen levels. You’re breathless even at rest. Many need oxygen therapy around the clock. Walking across a room can feel like running a marathon. This stage carries a high risk of respiratory failure, heart problems, and life-threatening flare-ups.
But here’s the thing: FEV1 doesn’t tell the whole story. Two people with the same FEV1 can feel completely different. One might still walk 5 miles a day. The other can barely get out of bed. That’s why doctors now also look at your symptoms and how often you have flare-ups to group you into A, B, C, or D - which directly affects your treatment plan.
Treatment by Stage: What Actually Works
Treatment isn’t one-size-fits-all. What helps in Stage 1 could be useless - or even harmful - in Stage 4.
Stage 1: Catch It Early
If you’re diagnosed here, time is your biggest ally. The single most effective thing you can do? Quit smoking. Studies show quitting at this stage can cut the rate of lung function decline by half. That’s not a small win - it’s life-changing.
Medication? Usually just a short-acting inhaler like albuterol, used only when you’re extra short of breath. No daily pills yet. But you should get your flu shot every year and consider the pneumococcal vaccine. These simple steps prevent infections that can wreck your lungs.
Stage 2: Building a Routine
This is where daily treatment begins. Long-acting bronchodilators - like tiotropium (Spiriva) or salmeterol (Serevent) - are prescribed to keep airways open all day. You’ll likely need one or two inhalers, taken every morning and sometimes at night.
Pulmonary rehabilitation is a game-changer. It’s not just exercise - it’s a 8- to 12-week program with trained therapists who teach you breathing techniques, safe physical activity, and how to manage your symptoms. People who complete it walk an average of 54 meters farther on a 6-minute walk test. That’s the difference between needing help to get to the bathroom and doing it on your own.
And yes - vaccines matter even more now. A bad cold can send you to the hospital.
Stage 3: Managing Flare-Ups
At this point, you’re probably on a combination inhaler - a long-acting beta-agonist (LABA) plus a long-acting muscarinic antagonist (LAMA). If you’ve had two or more flare-ups in a year, your doctor may add an inhaled steroid (ICS) to reduce inflammation.
Oxygen therapy may be introduced if your blood oxygen level drops below 88% at rest. This isn’t just for the end stage - it can improve energy, sleep, and even heart function. Portable oxygen tanks are bulky, but newer models are lighter and can run for 4-6 hours on a charge.
Many patients here start to feel anxious about leaving home. That’s normal. Pulmonary rehab can help rebuild confidence. And if you’re struggling with depression or panic attacks, talk to your doctor - mental health support is part of COPD care.
Stage 4: Living with Severe Limitations
Continuous oxygen therapy (15+ hours a day) becomes essential. Studies show it can improve survival by 44% in people with severe low oxygen levels.
Triple therapy - combining LABA, LAMA, and ICS in one inhaler - is now standard for those with frequent flare-ups. The FDA approved Breztri Aerosphere in September 2023 as the first single-inhaler triple therapy for COPD, making daily routines simpler.
Surgery? For a small group of patients, lung volume reduction surgery can remove the most damaged parts of the lung, giving the healthier parts room to expand. The NETT trial showed a 15% improvement in 2-year survival for eligible candidates.
Lung transplant is an option for those under 65 with FEV1 below 20% and no other major health problems. But it’s not for everyone - it’s a major operation with lifelong risks and strict eligibility rules.

What You’re Not Being Told: The Hidden Challenges
Medications are expensive. Spiriva costs $350-$400 a month without insurance. Many patients skip doses because they can’t afford them. Medicare covers 80% of oxygen costs after a $233 deductible, but portable units are still a hassle - they don’t last long, and you can’t always take them on planes or into restaurants.
And here’s the kicker: 70-80% of people use their inhalers wrong. If you’re not breathing in the right way, the medicine never reaches your lungs. That’s why you need a nurse or respiratory therapist to watch you use it - not just once, but multiple times. Most people need 3-5 sessions to get it right.
Adherence is another problem. Half of patients stop taking their daily meds within six months. Why? Side effects, complexity, or just forgetting. That’s why simplifying regimens - like switching to a single-inhaler triple therapy - is such a big deal.
What’s New in COPD Care (2025)
The field is moving fast. New drugs like ensifentrine - a once-daily inhaler that improves lung function by 13% - are showing promise in late-stage trials. Researchers are also exploring gene therapies and personalized treatments based on your unique lung biology.
Digital tools are helping too. The FDA-cleared Kyna COPD app tracks your symptoms daily and uses AI to predict a flare-up up to 7 days in advance with 82% accuracy. That means you can start treatment early - before you end up in the ER.
Telehealth is now standard. Most pulmonologists offer virtual check-ins, which makes follow-ups easier, especially for people who can’t travel far. In 2023, 62% of doctors used telehealth for COPD - up from just 15% in 2020.

Real People, Real Stories
On Reddit’s COPD community, one user wrote: “I had to quit my warehouse job at Stage 2. I couldn’t walk 200 feet without stopping.” Another said: “I can’t shower without oxygen. Brushing my teeth leaves me gasping.”
But there are wins too. A 2022 survey by the COPD Foundation found that 78% of people who completed pulmonary rehab said they could do daily tasks more easily. One woman in Brisbane, 68, started rehab after her Stage 3 diagnosis. She now walks her dog every morning - something she hadn’t done in two years.
What You Can Do Right Now
- If you smoke - quit today. There are free programs, patches, and medications that double your success rate.
- Get a spirometry test if you’re over 40 and have a smoking history or chronic cough.
- Ask your doctor about pulmonary rehab - it’s covered by Medicare and most private insurers.
- Learn how to use your inhaler correctly. Bring it to your next appointment and ask to demonstrate.
- Get vaccinated. Flu, pneumonia, and COVID-19 shots are not optional - they’re life-saving.
- Track your symptoms. Note when you feel more short of breath, when you cough more, or when your mucus changes color. This helps your doctor adjust your plan.
COPD doesn’t have to mean giving up your life. It means learning to live differently - and with the right tools, you can still do the things that matter.
Can COPD be reversed?
No, COPD cannot be reversed. The lung damage is permanent. But quitting smoking, using prescribed medications, and doing pulmonary rehab can slow the progression significantly - sometimes for decades. The goal is to preserve what’s left and prevent further decline.
Is COPD the same as asthma?
No. Asthma is usually reversible with medication and often starts in childhood. COPD is progressive, usually caused by long-term smoking, and typically appears after age 40. Some people have both - called asthma-COPD overlap syndrome - and need a different treatment approach.
How do I know if I’m having a COPD flare-up?
Signs include worsening shortness of breath, more frequent coughing, changes in mucus (color, thickness, or amount), increased wheezing, or feeling more tired than usual. If you notice these, contact your doctor right away. Early treatment can prevent a hospital visit.
Can I still exercise with COPD?
Yes - and you should. Exercise doesn’t make COPD worse; it helps your body use oxygen more efficiently. Start slow: walking for 5 minutes, twice a day. Work up to 30 minutes. Pulmonary rehab programs are designed specifically for people with COPD and are the safest way to begin.
What’s the life expectancy with COPD?
It varies widely. Someone with mild COPD who quits smoking can live for decades with a near-normal lifespan. Someone with severe COPD and frequent flare-ups may have a shorter life expectancy. But survival isn’t just about stage - it’s about how well you manage it. Staying active, avoiding infections, and following your treatment plan make a huge difference.
Is oxygen therapy addictive?
No. Oxygen is not addictive. It’s a treatment for low blood oxygen levels - not a drug. If you need it, your body is simply not getting enough on its own. Using oxygen as prescribed improves your quality of life and can help you live longer.
Can diet help with COPD?
Yes. Being underweight weakens your breathing muscles. Being overweight makes your lungs work harder. A balanced diet with enough protein, healthy fats, and vegetables helps maintain muscle strength and energy. Avoid bloating foods like carbonated drinks and beans if they make you feel fuller and more breathless.
Next Steps: What to Do Today
If you’ve been diagnosed with COPD, don’t wait. Schedule a pulmonary rehab referral. Ask your doctor for a spirometry test if you haven’t had one. Get your vaccines. Learn how to use your inhaler. Talk to someone who’s been through it - support groups are out there.
If you’re a smoker and haven’t been diagnosed yet - get tested. Early detection is the best defense. COPD doesn’t announce itself with a bang. It whispers. And if you listen - and act - you can still live well for a long time.
serge jane
Look I get that COPD is bad but let’s be real here the whole medical industrial complex is just milking this for profit. You think they really care if you live or die or do they just want you on inhalers forever so you keep buying them. I mean how many of these ‘new treatments’ are just repackaged old junk with a fancy name. And don’t even get me started on that Kyna app. AI predicting flare ups? Sounds like surveillance tech masquerading as healthcare. They’re tracking your breathing patterns now next thing you know your insurance will raise your rates because your ‘data profile’ says you’re high risk. This isn’t medicine it’s a data harvesting scheme with stethoscopes.
Sarah Swiatek
Wow. Just wow. You really think that’s how it works? That every doctor, every researcher, every nurse who’s spent decades studying this is just in it for the money? Come on. The fact that you’re so cynical about the system doesn’t make it evil it just makes you bitter. I’ve seen patients who quit smoking at Stage 1 and lived 20 more years with a good quality of life. I’ve seen people on oxygen who could finally hold their grandkids again. This isn’t about profit it’s about dignity. And yeah maybe some pharma companies are shady but the science behind pulmonary rehab? The 54-meter improvement? That’s real. That’s measurable. That’s human. Stop blaming the cure because the system is broken.
rob lafata
Oh honey you’re so naive. You think people with COPD are just sitting around waiting for their next inhaler? No. They’re drowning. In debt. In loneliness. In shame. I’ve watched my uncle go from fixing his own car to needing help to pee because his lungs gave out. And you wanna talk about ‘dignity’? What dignity is there when your inhaler costs more than your rent? When your portable oxygen tank gets confiscated at the airport because some TSA drone thinks it’s a bomb? When your wife leaves because you can’t even walk to the mailbox without wheezing like a broken bellows? This isn’t a textbook case. This is a slow-motion car crash and the system is the driver. And you? You’re just the passenger with a nice coat.
Rebecca Cosenza
My dad had COPD. Quit smoking. Did rehab. Lived 11 more years. Used his oxygen. Didn’t complain. Just lived. You’re right. It’s hard. But giving up hope doesn’t help. Just take the meds. Get the shot. Breathe.
Dave Wooldridge
EVERYTHING ABOUT COPD IS A LIE. The WHO? Controlled by Big Tobacco. The spirometry test? Calibrated to make smokers look sick. The ‘85-90% caused by smoking’ stat? Manufactured by the AMA to scare people into buying vape pens. I’ve been breathing clean air my whole life and I still wheeze. Why? Because the government is spraying chemtrails to thin the population. You think your oxygen tank is just for your lungs? Nah. It’s a tracker. They’re watching your exhales. They know when you sleep. When you eat. When you cry. And they’re coming for you next. Don’t trust the inhaler. Don’t trust the app. Don’t trust the nurse. Trust your gut. And if your gut says run… RUN.
Matthew McCraney
So let me get this straight. You’re telling me that if I just quit smoking and do some breathing exercises I won’t die? That’s rich. I’ve seen the ads. ‘COPD is manageable!’ Yeah right. Like obesity is manageable. Like poverty is manageable. Like being poor and old and broke in America is manageable. You think I don’t know people who died because they couldn’t afford Spiriva? You think I don’t know people who got denied oxygen because their ‘numbers’ weren’t bad enough? Don’t preach to me about ‘dignity’ when your insurance won’t cover the damn thing. I’m not mad at the disease. I’m mad at the people who let this happen.
Brianna Groleau
I’m from the Philippines and I’ve seen COPD up close. Not just from smoking. From cooking over wood fires. From living next to open-air junkyards. From kids breathing smog since they were born. We don’t have fancy inhalers or rehab centers. We have grandmas who walk with a cane and a plastic bag tied to their mouth to filter the dust. And they still smile. They still sing to their grandkids. They still clean the house even when they can’t catch their breath. I don’t know if the system is fair. But I know this: people don’t stop being human just because their lungs are broken. Maybe the real treatment isn’t in the medicine. Maybe it’s in remembering that we’re still here. Still trying. Still loving. Even when it hurts to breathe.
Nick Naylor
Let’s be clear: COPD is not a disease-it’s a behavioral failure. It’s a consequence of poor personal responsibility. Smoking is a choice. Air pollution exposure? Avoidable. Ignoring symptoms? Inexcusable. The medical establishment’s emphasis on ‘management’ and ‘rehabilitation’ is a euphemism for enabling laziness. You don’t get to smoke for 30 years and then expect society to subsidize your oxygen tank. The solution isn’t more drugs-it’s accountability. Mandatory smoking cessation programs. Financial penalties for non-compliance. Mandatory pulmonary rehab as a condition of insurance coverage. No more handouts. No more victim narratives. Just consequences. And if you can’t handle that? Then don’t complain when your lungs fail.
Rusty Thomas
Okay but like… I just watched this TikTok where this lady with Stage 3 COPD did a full yoga flow on oxygen and it was SO emotional?? Like she was crying and laughing and the music was ‘A Thousand Years’ and she finished by blowing a kiss to the camera?? I’m not even kidding. I cried. Like real tears. I just ordered a portable oxygen concentrator and I’m starting a COPD awareness channel. I’m gonna call it ‘Breathe With Me’ and we’ll do daily breathing challenges and I’ll interview people who still dance even when they’re wheezing. I need this in my life. Someone please help me make the logo. 🥺❤️🫁