When you're first told you have diabetes, the focus is often on blood sugar numbers. But soon after, the conversation turns to diabetes medications - and what they might do to your body. It’s not just about lowering glucose. It’s about understanding what you’re taking, what might go wrong, and how to handle it when it does.
Metformin: The First Line, But Not Always Easy
Most people with type 2 diabetes start with metformin. It’s cheap, effective, and has been around for decades. But for about one in three people, the side effects hit hard right away. Nausea, diarrhea, stomach cramps - these aren’t rare. In fact, a 2021 study in JAMA Internal Medicine found 26% of users had nausea, and 23% had diarrhea within the first month.
Many quit because of it. But here’s the trick: you don’t have to. Starting low - 500 mg once a day with dinner - and slowly increasing helps. Switching to the extended-release version cuts GI side effects by about half. And if it’s still too much, your doctor can adjust the timing or try another option.
There’s another hidden risk: vitamin B12 deficiency. After five or more years on metformin, up to 30% of people develop low B12 levels. That can mean fatigue, tingling in your hands and feet, or even memory problems. The fix? A simple blood test once a year. If levels are low, a monthly B12 shot or high-dose oral supplement usually fixes it in a few months.
Sulfonylureas: Effective, But Dangerous if You Skip a Meal
Drugs like glyburide and glipizide force your pancreas to pump out more insulin. They work - and they’re cheap. But they come with a big catch: low blood sugar. About 16% of people on these drugs have at least one serious low blood sugar episode each year. And it’s not just dizziness or sweating. Severe hypoglycemia can lead to seizures, falls, or even car accidents.
Why does this happen? It’s not just about taking too much. Skipping a meal, drinking alcohol, or exercising harder than usual can trigger it. Many people learn to fear it. A 2022 survey found 34% of insulin users intentionally underdose to avoid lows - and that’s a dangerous habit. The 15-15 rule helps: eat 15 grams of sugar (like juice or glucose tablets), wait 15 minutes, check your blood sugar again. Repeat if needed.
These drugs also cause weight gain - usually 2 to 4 kilograms. For someone trying to lose weight to manage diabetes, that’s frustrating. That’s why many doctors now avoid them unless other options aren’t working.
Thiazolidinediones: Powerfully Effective, But Risky for Some
Pioglitazone (Actos) makes your body respond better to insulin. It’s great for people with severe insulin resistance. But it comes with serious trade-offs. About 4-5% of users develop fluid retention, which can lead to swelling in the legs and, worse, heart failure. The PROactive trial showed a 43% higher risk of heart failure with this class.
Weight gain is common - 2 to 3 kg on average. Bone fractures, especially in women, are another concern. Because of these risks, doctors rarely prescribe these drugs anymore unless someone has no other options and no heart problems.

SGLT2 Inhibitors: New Kids on the Block
Drugs like Jardiance (empagliflozin), Farxiga (dapagliflozin), and Invokana (canagliflozin) work differently. They make your kidneys dump sugar out through urine. That lowers blood sugar - and helps you lose weight. Many people lose 2-5 kg in the first few months.
But they come with unique side effects. Genital yeast infections are common - affecting 10-15% of women and 3-5% of men. It’s not just itching. Some report painful urination or recurring infections. Simple fixes help: wash daily with mild soap, wear cotton underwear, avoid douches. Studies show this cuts recurrence by 60%.
There’s also a rare but dangerous risk: diabetic ketoacidosis (DKA). It’s not the same as the kind that happens when someone with type 1 diabetes misses insulin. This is “euglycemic DKA” - where blood sugar isn’t sky-high, but your body is still burning fat for fuel. Symptoms: nausea, vomiting, stomach pain, confusion. It’s often missed because glucose levels look normal. If you feel unwell while on these drugs, check for ketones with a urine strip or blood meter.
Urinary tract infections and dehydration are also more common. Drink plenty of water. If you’re sick, vomiting, or sweating a lot, talk to your doctor about holding the dose temporarily.
GLP-1 Receptor Agonists: Weight Loss That Works - But Stomach Pain Too
These injectables - like Ozempic, Victoza, and Mounjaro - are changing the game. They slow digestion, reduce appetite, and boost insulin only when needed. The result? Better blood sugar control and real weight loss. In one trial, people lost over 5 kg in six months.
But the side effects are real. Nausea hits 30-50% of users. Vomiting and diarrhea are common too. Most people get used to it after a few weeks. Starting low and going slow helps. Many doctors now begin with half the dose for the first month.
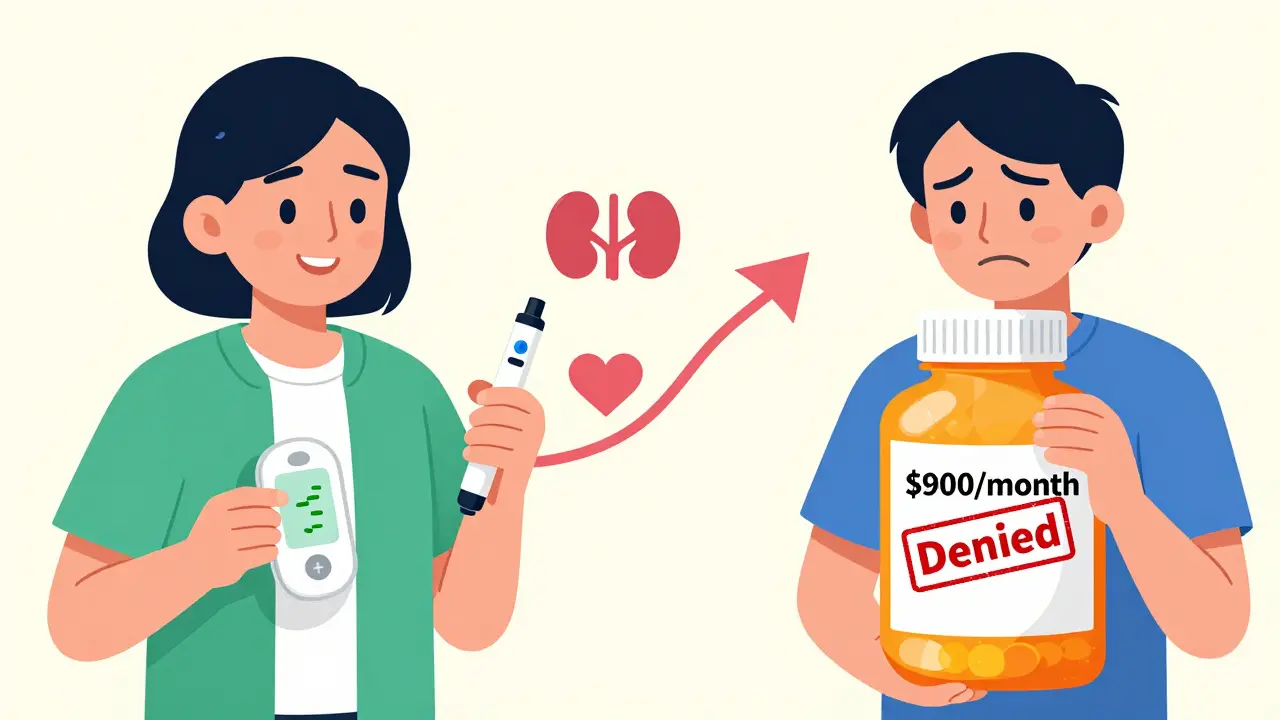
There’s also a risk of gallbladder disease and, rarely, pancreatitis. If you have severe, constant stomach pain that doesn’t go away, get it checked. And while these drugs are great for weight loss, they’re expensive - often over $900 a month without insurance. Many people can’t afford them long-term.
Insulin: The Most Powerful - and Most Feared
Insulin is the only option for type 1 diabetes. Many with type 2 eventually need it too. It’s the most effective at lowering blood sugar. But it’s also the most dangerous if misused.
Low blood sugar is the biggest fear. People on intensive insulin therapy can have 15 to 30 episodes of hypoglycemia per year. That’s why many avoid taking it as prescribed. Fear becomes a barrier to control.
Weight gain is another issue. Insulin tells your body to store fat. Most gain 2 to 5 kg when starting. But it’s not inevitable. Pairing insulin with GLP-1 agonists or SGLT2 inhibitors can help limit weight gain.
Injection site reactions - redness, lumps, pain - happen too. Rotating sites helps. And if you’re on multiple daily injections, consider a pump or a smart pen with dose tracking. Continuous glucose monitors (CGMs) cut severe lows by 40%, according to the DIAMOND trial.
What’s Changing Right Now?
The diabetes drug market is shifting fast. Sulfonylureas are fading. SGLT2 inhibitors and GLP-1 agonists are rising. Why? Because they don’t just lower sugar - they protect your heart and kidneys. The EMPA-KIDNEY trial showed empagliflozin slowed kidney disease progression even in people without diabetes.
New drugs like tirzepatide (Mounjaro) combine two hormones (GIP and GLP-1) and are causing bigger weight loss with less nausea than older GLP-1 drugs. Oral versions of GLP-1 drugs are coming soon - no more needles.
But access remains a huge problem. One in four Americans with diabetes skip doses because they can’t afford them. Generic metformin costs $4 a month. Newer drugs can cost over $900. Insurance doesn’t always cover them, even if they’re medically right.
What Should You Do?
There’s no one-size-fits-all. Your best medication depends on your weight, heart health, kidney function, budget, and how you feel day to day.
- If you’re overweight and have heart or kidney disease: SGLT2 inhibitors or GLP-1 agonists are likely your best bet.
- If you’re young, healthy, and on a budget: Metformin is still the go-to.
- If you’ve had low blood sugar before: Avoid sulfonylureas.
- If you’re afraid of needles: Ask about oral options or newer GLP-1 pills coming in 2025.
Side effects don’t mean you have to quit. They mean you need to talk to your doctor - and adjust. Many side effects fade. Many can be managed. And many can be avoided with the right start.
Your goal isn’t just to take pills. It’s to live well - without fear, without pain, without constant low blood sugar. That’s possible. But it takes knowing what you’re on - and speaking up when something doesn’t feel right.
What are the most common side effects of metformin?
The most common side effects are nausea, diarrhea, stomach cramps, and loss of appetite. These affect 20-30% of users, especially when starting. Taking it with food, starting with a low dose, or switching to extended-release form can reduce these effects by up to 50%. Long-term use may lower vitamin B12 levels, so annual blood tests are recommended.
Can diabetes medications cause weight gain?
Yes, some do. Insulin, sulfonylureas, and thiazolidinediones (like pioglitazone) commonly cause weight gain - usually 2 to 5 kg. SGLT2 inhibitors and GLP-1 agonists, however, often lead to weight loss. If weight is a concern, your doctor can choose medications that help you lose or at least not gain weight.
Why do SGLT2 inhibitors cause yeast infections?
These drugs make your kidneys remove sugar through urine. That sugar ends up in your genital area, creating a moist, sugary environment where yeast thrives. Women are more affected than men. Keeping the area clean and dry, wearing cotton underwear, and avoiding scented products can reduce infection risk by 60%. If infections recur, talk to your doctor about antifungal treatments or adjusting your medication.
Is it safe to take diabetes meds during pregnancy?
Metformin is the only oral diabetes medication generally considered safe during pregnancy (FDA Category B). Insulin is the standard treatment for gestational diabetes and type 1 or 2 diabetes in pregnancy. Most other oral drugs - including SGLT2 inhibitors and GLP-1 agonists - are not recommended due to unclear fetal risks. Always consult your doctor before getting pregnant if you’re on diabetes medication.
What should I do if I experience low blood sugar?
Use the 15-15 rule: consume 15 grams of fast-acting sugar - like 4 ounces of juice, 3-4 glucose tablets, or 1 tablespoon of honey. Wait 15 minutes, then check your blood sugar. If it’s still below 4 mmol/L, repeat. Once your sugar is back up, eat a small snack with protein or carbs to prevent another drop. If you’re confused, unconscious, or having seizures, someone must give you glucagon or call emergency services immediately.
Are newer diabetes drugs worth the cost?
For many, yes - especially if you have heart disease, kidney disease, or need to lose weight. GLP-1 agonists and SGLT2 inhibitors reduce the risk of heart attacks, strokes, and kidney failure by up to 38%. While they cost more than metformin ($900 vs. $4 a month), they can save money long-term by preventing hospitalizations and complications. Ask about patient assistance programs, generic options, or insurance appeals if cost is a barrier.

Martin Viau
Metformin is literally the only reason I'm not on insulin. But that GI hell? Pure torture. I went from 500mg once to 850mg twice and thought I was gonna die. Extended-release saved my ass. Also, B12 deficiency? Real. My neurologist caught it after 7 years of tingling hands. Shot every month now. No more brain fog. If you're on this for 5+ years, get tested. Seriously.
Also, why are we still talking about sulfonylureas? They're ancient. Like, 'I got this in 1998' ancient. If your doc still prescribes glyburide, ask for a second opinion. Hypoglycemia ain't a side effect - it's a liability.
Robb Rice
Thank you for this detailed breakdown. I appreciate the clinical accuracy and the emphasis on patient-centered management. While metformin remains first-line, the evolving evidence around SGLT2 inhibitors and GLP-1 agonists is compelling - particularly for those with comorbid cardiovascular or renal disease. The cost barrier, however, remains a systemic failure. Insurance formularies should prioritize outcomes over profit margins.
Also, the mention of euglycemic DKA is critical. Many providers overlook this. Patients need to be educated on ketone testing during illness, even if glucose levels appear normal.
Harriet Hollingsworth
So let me get this straight - people are okay with taking drugs that cause yeast infections and heart failure just so they can lose a few pounds? That’s not medicine, that’s vanity. And now we’re telling diabetics to just ‘drink more water’ when their kidneys are dumping sugar like a toilet with a leak? This is what happens when pharma runs the show. You’re not fixing diabetes - you’re just making money off the symptoms.
Deepika D
Hey everyone - I’ve been living with type 2 for 14 years and I want to say this: you are NOT alone. I started on metformin and thought I’d never make it past week one - nausea, cramps, the whole thing. But I started at 500mg once a day with dinner, stayed there for two weeks, then went up slowly. Now I’m on 1000mg ER and feel great.
Also - B12! I didn’t know mine was low until I started getting dizzy and my hands felt like they were asleep. Blood test = $20. B12 shot = $15. Game changer.
And for those scared of GLP-1s? Start at half dose. Give it 4 weeks. Nausea fades. I lost 18 lbs and my A1c dropped from 8.1 to 5.9. It’s not magic - it’s science. And yes, it’s expensive - but ask your pharmacy about patient assistance. I got mine for $25/month through the manufacturer’s program. You’ve got this. 💪❤️
Bennett Ryynanen
Y’all act like metformin is the devil. Bro, I’ve been on it for 10 years. Nausea? Yeah, first week. Diarrhea? Maybe. But I’m alive. My A1c is 5.7. I don’t need insulin. I don’t need shots. I don’t need to cry in the bathroom every time I eat. You want to complain? Go live on insulin with 3 daily shots and a pump and see how much you like it.
And SGLT2s? I had a yeast infection once. Used Monistat. Done. Not a crisis. You think your body’s gonna break because you pee out sugar? Nah. It’s just your kidneys doing their job. Stop being dramatic.
Chandreson Chandreas
Life’s weird, right? 🤔
Metformin gave me the runs but also gave me back my energy. SGLT2s gave me yeast infections but also made my jeans fit better. GLP-1s made me puke for a week but now I don’t crave pizza at 2am.
It’s not about the pills. It’s about the life after the pills. I used to be scared of my own body. Now I just listen. And sometimes, I pee sugar. And that’s okay. 🌱💧
Also - B12 test. Do it. It’s like checking your tire pressure. No one tells you to, but you should.
Darren Pearson
It is both intellectually and ethically irresponsible to reduce complex metabolic pathophysiology to a mere pharmacological checklist. The paradigmatic shift toward SGLT2 inhibitors and GLP-1 receptor agonists reflects not merely therapeutic efficacy, but a broader epistemological reorientation in endocrinology - one that prioritizes organ protection over glycemic reduction alone.
Furthermore, the economic disparity in access to these agents underscores a systemic failure of healthcare policy in the United States, wherein cost-containment measures supersede evidence-based clinical outcomes. One must question the moral architecture of a system that permits a $4 generic to remain the default while life-altering therapeutics are priced beyond the reach of the very population they are designed to serve.
Stewart Smith
Wow. So metformin gives you diarrhea, GLP-1s give you nausea, SGLT2s give you yeast infections, and insulin gives you weight gain… and we’re supposed to be grateful?
Someone get me a crystal ball - because I need to know which side effect I’m gonna get next. Maybe my kidneys will start singing show tunes? 🎤
At this point, I’m just waiting for the pill that makes you lose weight, cure your diabetes, and also text your mom to remind you to take it.
Retha Dungga
we are all just trying to survive the machine
metformin is the only thing keeping me from being a ghost
but i still cry sometimes when i see the price of my new meds
why does healing cost so much
and why do they make us feel guilty for wanting to live
❤️
Jenny Salmingo
I’m from the Philippines and my dad’s been on metformin for 15 years. He never had side effects because he took it with rice and fish every night. No fancy tricks - just food, patience, and a doctor who listened.
Also - B12? He got it from eggs and milk. No shots. Just ate. Maybe we’re overcomplicating this? Sometimes the simplest things work best.
And yes - if you can’t afford the new drugs, don’t panic. Metformin still saves lives. You’re not failing if you’re on the old stuff.
Aaron Bales
Start low, go slow with metformin. Extended-release cuts GI issues in half. Test B12 yearly. Avoid sulfonylureas if you’ve had lows. SGLT2s? Watch for DKA - check ketones if you’re sick. GLP-1s? Nausea fades. Weight loss helps. Insulin? Use a CGM. Done. No drama. Just facts.
Lawver Stanton
Let’s be real - this whole thing is a corporate circus. Metformin? Cheap. Safe. Effective. But it’s not sexy. So the pharma giants spent billions marketing SGLT2s and GLP-1s like they’re miracle weight-loss potions. They’re not. They’re just slightly better at protecting your heart - and way better at making shareholders rich.
And don’t get me started on the ‘euglycemic DKA’ nonsense. You’re telling me someone can be in diabetic ketoacidosis and their blood sugar looks normal? That’s not medicine - that’s a diagnostic trap designed to keep people coming back for more tests, more strips, more $900 prescriptions.
Meanwhile, the guy who can’t afford $4 metformin is told to ‘just eat better’ while his insurance denies him the drug that keeps him alive. This isn’t healthcare. It’s capitalism with a stethoscope.
Sara Stinnett
How quaint. You treat diabetes like a math problem - take pill A, get result B. But the body isn’t a spreadsheet. It’s a symphony of chaos, trauma, and inherited grief. You speak of ‘side effects’ as if they’re glitches - when in truth, they are the body screaming. Nausea isn’t an inconvenience - it’s your gut rejecting the chemical assault. Yeast infections? Your microbiome crying for mercy. Weight gain? Your cells begging for safety after years of metabolic betrayal.
And you think a $4 generic fixes this? No. You’re patching a wound with duct tape and calling it healing. The real cure isn’t in a pill - it’s in dismantling the systems that made you sick in the first place: poverty, processed food, stress, and the lie that health is a personal responsibility.
Until we address that, you’re just rearranging deck chairs on the Titanic. And yes - I’m still on metformin. But I’m not fooled.