When someone has a seizure, it’s not just a moment of confusion or convulsions-it’s often the first sign of something deeper. Epilepsy isn’t a single condition. It’s a group of neurological disorders where the brain’s electrical activity goes off-track, leading to repeated seizures. The good news? We now understand it better than ever. The bad news? Many people still get misdiagnosed, sometimes for years. If you or someone you care about has had a seizure, knowing the difference between seizure types, what sets them off, and how medications actually work can make all the difference.
What Counts as Epilepsy? It’s Not Just One Seizure
A single seizure doesn’t mean you have epilepsy. That’s a common misunderstanding. According to the International League Against Epilepsy (ILAE), epilepsy is diagnosed when you’ve had at least two unprovoked seizures more than 24 hours apart. Or, if you’ve had one seizure and tests show you have a 60% or higher chance of having another. This isn’t just paperwork-it changes how doctors treat you. If you’ve had a seizure after a head injury, high fever, or alcohol withdrawal, that’s a provoked seizure. It’s not epilepsy. But if your brain keeps misfiring without an obvious trigger, that’s when the diagnosis of epilepsy comes in.
Worldwide, about 50 million people live with epilepsy. In the U.S., that’s 3.4 million. And every year, 5 million more are diagnosed. The numbers are big, but the confusion around diagnosis is bigger. Studies show 15-20% of people are misclassified at first. Many think they have generalized epilepsy when it’s actually focal. Others are told they have epilepsy when it’s something else entirely-like psychogenic non-epileptic seizures (PNES), which look like epileptic seizures but aren’t caused by abnormal brain electricity. PNES affects 20-30% of patients sent to epilepsy monitoring units. Getting it right matters because the treatment is completely different.
The New Seizure Classification: Simpler, But Still Complex
In 2025, the ILAE updated its seizure classification system-and it’s a big deal. They cut the number of named seizure types from 63 down to 21. Why? Because doctors were drowning in names. The old system had too many labels for things that looked similar. The new one focuses on what matters most: where the seizure starts and what it does.
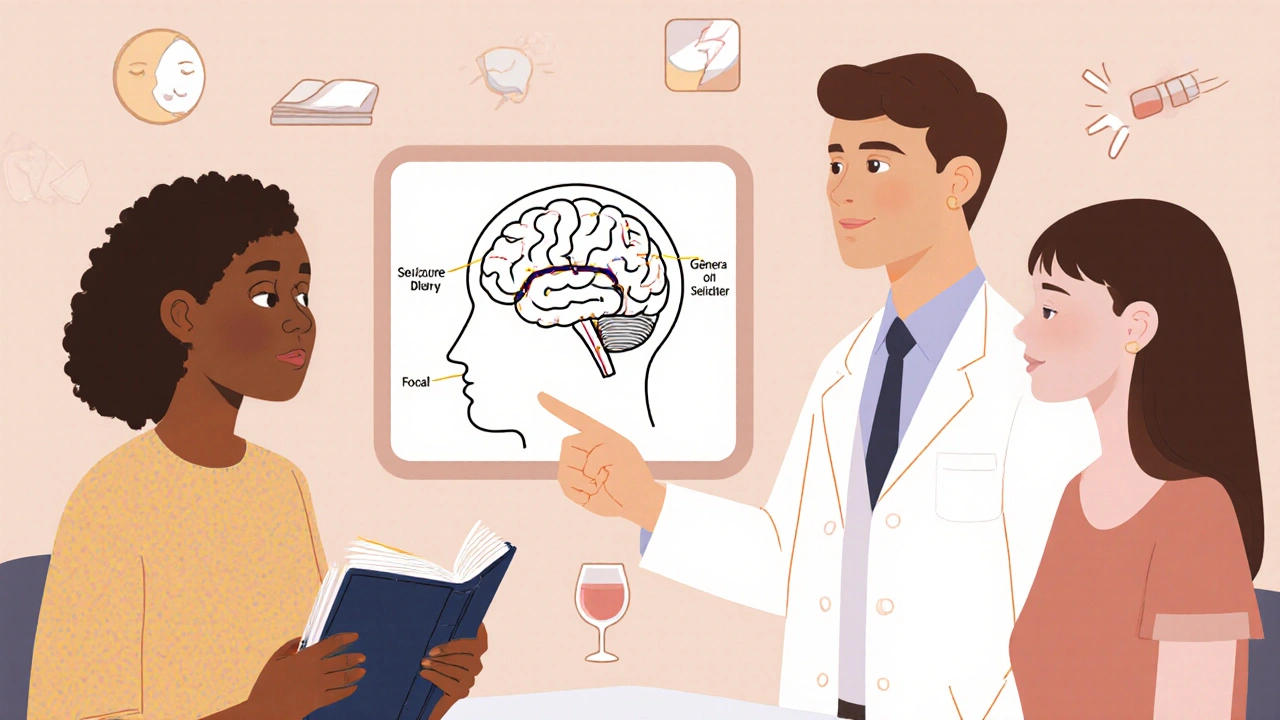
There are now four main seizure categories:
- Focal seizures - start in one part of the brain
- Generalized seizures - involve both sides of the brain from the start
- Unknown onset - you don’t know where it began
- Unclassified - not enough info to tell
Focal seizures are the most common, making up about 60% of all epilepsy cases. They split into two subtypes based on consciousness:
- Aware - you’re fully conscious during it. You might feel a strange smell, see flashing lights, or have a rising feeling in your stomach. These used to be called “simple partial” seizures.
- Impaired awareness - you lose some level of awareness. You might stare blankly, fumble with your clothes, or repeat words without meaning to. These were once called “complex partial.” About 75% of focal seizures fall into this group.
Generalized seizures are less common but harder to miss. They include:
- Absence seizures - brief staring spells, often in children. Lasts 5-10 seconds. Used to be called “petit mal.”
- Myoclonic seizures - sudden jerks in arms or legs. Often happens right after waking up.
- Tonic-clonic seizures - the classic “grand mal.” Body stiffens, then jerks. You lose consciousness. This is what most people picture when they think of epilepsy.
- Atonic seizures - sudden loss of muscle tone. You might drop to the floor without warning.
- Tonic and clonic - less common alone, but parts of tonic-clonic seizures.
One major change? The term “motor” vs. “non-motor” is gone. Now it’s “observable” vs. “non-observable.” Why? Because some seizures don’t have visible signs. You might feel a wave of fear, hear voices, or lose your sense of time-but look perfectly normal. These were often missed before.
What Triggers Seizures? It’s Not Just Stress
People often think seizures happen for no reason. But most have triggers. And knowing yours can cut down on episodes dramatically.
Common triggers include:
- Sleep deprivation - the #1 trigger. Missing even one night of sleep can spike seizure risk.
- Alcohol and drug use - not just binge drinking. Even moderate alcohol can interfere with meds.
- Flashing lights - affects about 3% of people with epilepsy. Not as common as people think, but real.
- Missed medications - skipping even one dose increases risk by 30-50%.
- Hormonal changes - many women have more seizures around their period. This is called catamenial epilepsy.
- Stress and anxiety - not the cause, but a powerful amplifier.
- Illness and fever - especially in kids.
One study found that people who tracked their triggers and avoided them reduced seizures by 40% in six months. It’s not magic. It’s management. Keep a simple log: what you ate, how much you slept, your stress level, and when seizures happened. Patterns show up fast.

Antiepileptic Medications: How They Work and What to Expect
There are over 30 FDA-approved antiepileptic drugs (AEDs). No single one works for everyone. The goal isn’t to eliminate all seizures-though that’s ideal. It’s to find the right balance: fewer seizures, fewer side effects.
First-line drugs for focal seizures include:
- Lamotrigine - good for mood stability, slow titration needed
- Levetiracetam - fast-acting, few interactions, common in kids
- Carbamazepine - effective but needs blood tests to monitor levels
- Valproate - powerful but risky in women of childbearing age due to birth defects
For generalized seizures, especially absence or myoclonic:
- Ethosuximide - first choice for absence seizures
- Valproate - broad spectrum, works for multiple types
- Topiramate - can cause weight loss and cognitive fog
Side effects are real. Dizziness, fatigue, weight gain, memory issues, rashes. Some people stop taking meds because of them. But here’s the thing: stopping without medical advice is dangerous. It can lead to status epilepticus-a life-threatening seizure that won’t stop.
Medication success rates vary. About 70% of people become seizure-free with the first or second drug. The other 30% have drug-resistant epilepsy. For them, options include surgery, vagus nerve stimulation, or dietary therapies like the ketogenic diet. But meds are still the starting point for nearly everyone.
Why Getting the Classification Right Changes Everything
Here’s the bottom line: if your seizure type is misclassified, you’re likely on the wrong medication. A 2023 study found that 27% of people were prescribed meds that didn’t match their seizure type. That’s not just ineffective-it’s harmful. Giving a drug for generalized seizures to someone with focal epilepsy can make things worse.
Take absence seizures. If a doctor mistakes them for daydreaming or ADHD, the child gets stimulants instead of ethosuximide. The seizures keep happening. School performance plummets. Parents feel like they’re failing.
Or consider focal seizures with impaired awareness. If they’re labeled as “psychogenic,” the person gets therapy instead of antiepileptic drugs. The seizures continue. The stigma grows. They’re told it’s “all in their head.” But it’s not. It’s a brain disorder.
Accurate classification leads to better outcomes. One study showed patients with correctly classified seizures were 34% more likely to stick with their meds. Why? Because they understood what was happening. They weren’t just taking pills-they were managing a condition they finally understood.

What’s Next? AI, Genetics, and Better Tools
The future is coming fast. The ILAE is developing an AI tool to help classify seizures from video recordings. Early tests show it improves accuracy by 18% for non-specialists. That’s huge for rural clinics or countries without neurologists.
Genetics is also changing the game. We now know specific gene mutations link to certain epilepsy syndromes. In the next five years, genetic testing may become standard for children with early-onset epilepsy. That could mean personalized meds before trial-and-error.
And the tools are getting smarter. Wearables that detect abnormal movement or heart rate changes during seizures are now FDA-approved. Some can alert caregivers in real time. That’s not sci-fi-it’s here.
But none of this matters if the basics aren’t covered. You still need a clear history, a good EEG, and a doctor who listens. Too often, patients are rushed. Seizures are dismissed. Misclassification continues.
If you’ve been told you have epilepsy-or if you’ve had a seizure-ask: What type is it? What’s the evidence? What’s the plan? Don’t accept a label without understanding it. Your brain deserves better.
Can you outgrow epilepsy?
Yes, many children outgrow epilepsy, especially those with absence seizures or benign rolandic epilepsy. Around 70% of children with epilepsy become seizure-free within 10 years, even without medication. But for adults, especially those with brain injuries or structural abnormalities, epilepsy is usually lifelong. It depends on the cause, not just the age.
Are seizures always noticeable?
No. Many seizures have no visible signs. You might feel a strange taste, have a sudden sense of dread, or lose track of time for a few seconds. These are called non-observable focal seizures. They’re easy to miss-both by others and sometimes by the person experiencing them. That’s why eyewitness accounts and EEGs are so important.
Do antiepileptic drugs cure epilepsy?
No. AEDs control seizures but don’t cure the underlying condition. They work by stabilizing brain activity. If you stop taking them, seizures often return. Some people can eventually taper off after being seizure-free for 2-5 years, but that’s decided carefully with a neurologist. It’s not a guarantee.
Can stress cause epilepsy?
Stress doesn’t cause epilepsy, but it can trigger seizures in people who already have it. Chronic stress raises cortisol levels, which can lower the seizure threshold. Managing stress through sleep, therapy, or mindfulness doesn’t cure epilepsy, but it can reduce how often seizures happen.
Is epilepsy genetic?
Some forms are. About 30-40% of epilepsy cases have a genetic component. This includes syndromes like Dravet syndrome or juvenile myoclonic epilepsy. But most cases aren’t inherited. Trauma, stroke, infections, or brain tumors are more common causes in adults. Genetic testing is becoming more common, especially for children with early-onset seizures.
What should I do if someone is having a seizure?
Stay calm. Time the seizure. If it lasts more than 5 minutes, or if the person has another one right after, call emergency services. Don’t put anything in their mouth. Turn them gently onto their side to keep the airway clear. Remove nearby objects. Stay with them until they’re fully awake. Most seizures end on their own. Your calm presence is the most important thing.
Can you drive if you have epilepsy?
It depends on your country’s laws and your seizure control. In Australia, you must be seizure-free for 6 months (or 3 months if only during sleep) before driving. Rules vary by state. In the U.S., it’s state-specific but usually requires 3-12 months seizure-free. Always check with your doctor and local transport authority. Driving with uncontrolled seizures puts you and others at serious risk.
Final Thoughts: Knowledge Is Your Best Medicine
Epilepsy isn’t a life sentence. But it’s not something you can ignore either. The right diagnosis, the right meds, and the right support can let you live a full life. The new classification system isn’t just for doctors-it’s for you. If you understand whether your seizures are focal or generalized, if you know your triggers, and if you know how your meds work, you’re not just a patient. You’re a partner in your care.
Don’t let confusing terms or outdated info hold you back. Ask questions. Keep a seizure diary. Find a neurologist who listens. And remember: you’re not alone. Millions are walking this path. The tools are better. The understanding is deeper. And with the right information, you can take back control.
Alex Ramos
Man, this post hit different. I’ve had focal impaired awareness seizures since I was 16, and no one ever explained it like this. That bit about non-observable seizures? Yeah, I’ve had those. Just felt like time froze for 10 seconds, no one noticed, I thought I was zoning out. Turns out it was my brain glitching. 😅 Got my diagnosis after 5 years of being called ‘distracted.’ This info could save someone’s life.
Johnson Abraham
lol so now we got 21 types of seizures? next theyll say theres a subtype for when u sneeze during one. also valproate causes birth defects? wow shocker. so women just cant have epilepsy? guess we should ban em from meds too 😂
Shante Ajadeen
Thank you for writing this. I’m a mom of a kid with absence seizures, and I’ve been so lost. The part about mistaking them for ADHD? That’s us. We went down that road for a year. When the neurologist finally said ‘it’s not inattention, it’s epilepsy’ - I cried. This post feels like a hug. Please share it with every pediatrician you know.
dace yates
Wait - if non-observable seizures are so common, why aren’t they better documented in EEG protocols? Most clinics only look for motor signs. What about the people who just feel ‘off’ or get sudden nausea? Is there data on how many get misdiagnosed because their seizures aren’t ‘visible’ enough?
Danae Miley
The ILAE’s 2025 classification update is a monumental improvement, but the article fails to address the systemic failure in primary care. General practitioners still diagnose epilepsy based on anecdotal reports, not EEGs or video telemetry. Until we mandate neurology referrals after the first unprovoked seizure, misclassification rates won’t drop. This isn’t just about terminology - it’s about access to diagnostics.
Charles Lewis
It is imperative to underscore the profound societal implications of accurate epilepsy classification. When individuals are misdiagnosed with psychogenic non-epileptic seizures, they are often subjected to stigmatizing psychological evaluations that neglect the biological underpinnings of their condition. This misattribution not only delays appropriate pharmacological intervention but also reinforces harmful narratives that frame neurological disorders as psychological failures. The integration of AI-assisted video analysis, as mentioned, represents a critical step toward democratizing diagnostic precision - particularly in underserved regions where neurologists are scarce. However, we must couple technological innovation with robust training for frontline clinicians, ensuring that diagnostic tools are not merely adopted but understood. Epilepsy is not a monolith, and our response must reflect that complexity with both scientific rigor and human empathy.
Renee Ruth
So let me get this straight - you’re telling me someone can have a seizure and not even know it? And doctors just… miss it? That’s insane. I knew a girl in college who kept ‘spacing out’ and everyone thought she was high. Turns out she had seizures. Her parents didn’t believe her until she collapsed at a party. Now she’s on meds and they’re all like ‘oh we should’ve known.’ NO. YOU SHOULDN’T HAVE. THIS IS A SYSTEMIC FAILURE. 😭
David Barry
US doctors overdiagnose epilepsy. In Australia we wait for 2 seizures + EEG confirmation before even calling it epilepsy. Here? One weird episode and they’re writing scripts for lamotrigine. My cousin got misdiagnosed because she had a panic attack during a migraine. Now she’s on 3 meds and can’t drive. This isn’t medicine. It’s liability insurance.
Alyssa Lopez
Why are we letting big pharma push these AEDs? Valproate? Toxic. Levetiracetam? Makes people suicidal. Lamotrigine? Rashes. We need natural cures. CBD oil, keto diet, no sugar. Why are we poisoning people? The government is in bed with the drug companies. Wake up. Epilepsy is a spiritual imbalance - not a chemical one.
edgar popa
my bro had a seizure at work last year. they thought he was drunk. he wasnt. he’s fine now on levetiracetam. this post is legit. thx for sharing. 🙌
Eve Miller
It’s irresponsible to suggest that people can ‘outgrow’ epilepsy without emphasizing that this only applies to specific syndromes in children - not adults with acquired brain injuries. This oversimplification risks encouraging patients to discontinue treatment prematurely. The phrase ‘many children outgrow it’ is dangerously misleading without context. Epilepsy is not a phase. It is a chronic neurological condition requiring lifelong vigilance - even when seizures are controlled.
Chrisna Bronkhorst
They say stress doesn't cause epilepsy but it sure as hell makes it worse. My sister had 3 seizures in one week after her mom died. No meds changed. Just stress. Then she started yoga and stopped having them. No drugs. Just peace. Maybe we need to stop treating the brain like a broken circuit and start treating the person like a whole human.