Anxiety-Addiction Risk Assessment Tool
This assessment tool will help you understand your risk of developing substance use disorder as a result of anxiety. The questions are based on the content from the article about anxiety and addiction.
Anxiety Symptoms
Substance Use Patterns
Coping Strategies
Your Risk Assessment
When anxiety starts pulling the strings of daily life, many people look for quick relief. Unfortunately, that relief often comes in the form of substances that promise a temporary calm - and before you know it, a pattern of dependence can emerge. Understanding anxiety and addiction isn’t just a medical exercise; it’s the first step toward breaking a cycle that affects millions worldwide.
What Exactly Is Anxiety?
Anxiety is a persistent feeling of worry, tension, or unease that can interfere with everyday activities. It shows up as racing thoughts, a knot in the stomach, or a constant sense that something bad is about to happen. While occasional nervousness is normal, chronic anxiety can become a diagnosable disorder, such as Generalized Anxiety Disorder (GAD) or Panic Disorder.
Defining Addiction in Simple Terms
Addiction refers to a compulsive, repeated use of a substance or behavior despite harmful consequences. It’s not just about the substance; it’s about the brain’s reward system being hijacked, leading to cravings, loss of control, and withdrawal when the substance is stopped.
Why Anxiety and Addiction Often Walk Hand‑in‑Hand
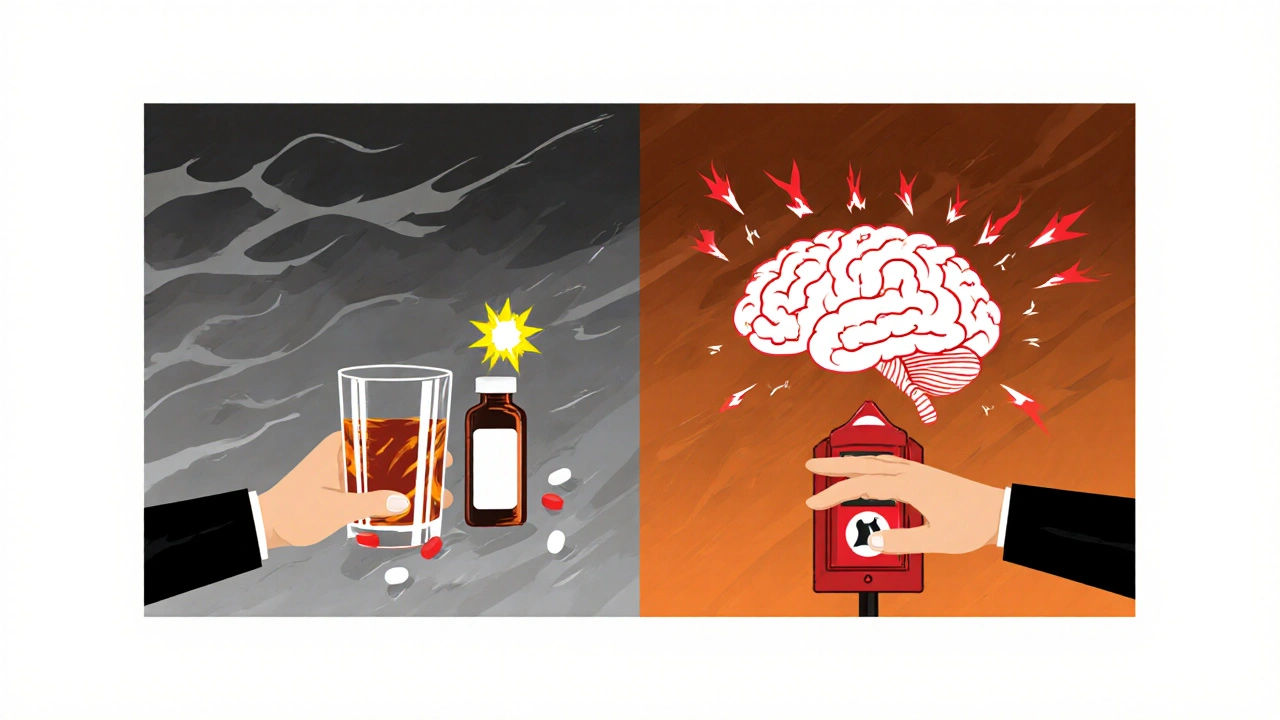
Think of anxiety as a fire alarm that never stops ringing. The body releases stress hormones like cortisol, and the brain’s neurotransmitter balance goes haywire. To silence that alarm, many turn to alcohol, prescription meds, or illicit drugs. These substances can temporarily lower the alarm’s volume by flooding the brain with dopamine, the "feel‑good" chemical.
When this pattern repeats, the brain rewires itself. What began as a coping trick becomes a habit, and then a dependence. This is called the Substance Use Disorder a medical condition characterized by an uncontrolled use of substances despite harmful outcomes.
Common Substances People Use to Self‑Medicate
- Alcohol - depresses the central nervous system and can mask racing thoughts for a short period.
- Opioids - provide powerful pain relief and a calming effect, but quickly lead to tolerance and dependence.
- Prescription benzodiazepines (e.g., Xanax, Valium) - directly target anxiety pathways but carry high addiction risk.
- Nicotine - its stimulant effect can feel soothing when anxiety spikes, yet it reinforces the stress‑relief loop.
How the Brain’s Chemistry Fuels the Cycle
Two neurotransmitters dominate this conversation: Dopamine a chemical that signals pleasure and reward in the brain and Stress the physiological response that releases cortisol and prepares the body for "fight or flight". When you use a substance, dopamine spikes, creating a brief sense of relief. The brain then learns, "If I’m anxious, I should reach for that substance." Over time, natural dopamine production can dip, leaving you feeling more anxious when you’re not using the substance - a perfect self‑reinforcing loop.
Spotting the Warning Signs Early
Recognizing the connection early can save you from a deeper plunge. Look out for these red flags:
- Increased use of alcohol or drugs specifically after stressful or anxious events.
- Needing larger amounts to achieve the same calming effect (tolerance).
- Feeling irritable, shaky, or sleepless when you try to cut back.
- Neglecting responsibilities - work, school, or relationships - because of substance use.
- Hiding or lying about how much you’re using.
Effective Strategies to Break the Cycle
There’s no one‑size‑fits‑all answer, but blending mental‑health care with addiction treatment yields the best outcomes.
1. Talk Therapy - The Backbone of Recovery
Cognitive Behavioral Therapy a structured, short‑term therapy that helps identify and change negative thought patterns is especially powerful. CBT teaches you to recognize anxiety triggers, challenge catastrophic thoughts, and replace them with healthier coping mechanisms.
2. Medication - When the Brain Needs a Reset
Selective serotonin reuptake inhibitors (SSRIs) or serotonin‑norepinephrine reuptake inhibitors (SNRIs) can reduce both anxiety and the urge to self‑medicate. However, they must be prescribed carefully, especially if you’re already using substances that affect the same pathways.
3. Peer Support - You’re Not Alone
12‑step groups, SMART Recovery, or community counseling circles provide accountability and shared experiences. Hearing how others navigated the anxiety‑addiction link can boost motivation.
4. Lifestyle Tweaks - Small Changes, Big Impact
- Regular physical activity - boosts endorphins, reduces cortisol.
- Mindfulness meditation - trains the brain to observe anxiety without reacting.
- Consistent sleep schedule - restores neurotransmitter balance.
- Balanced nutrition - stabilizes blood sugar, which can affect mood swings.
Comparison Table: Common Anxiety‑Driven Substances and Targeted Interventions
| Trigger | Typical Substance | Primary Symptoms | Recommended Intervention |
|---|---|---|---|
| Social anxiety | Alcohol | Shaky hands, rapid heart rate, avoidance | CBT for social skills, SSRIs, peer‑support groups |
| Chronic stress | Opioids | Constipation, drowsiness, intense cravings | Medication‑assisted treatment (MAT), stress‑management training |
| Insomnia | Benzodiazepines | Daytime fatigue, memory gaps, dependence | Sleep hygiene, CBT‑I (insomnia), gradual tapering under medical supervision |
| Generalized anxiety | Nicotine | Rapid breathing, irritability, frequent breaks | Nicotine replacement therapy, mindfulness, SSRIs |
Common Misconceptions That Can Stall Recovery
Myth 1: "If I’m not drinking or using drugs, my anxiety will disappear."
Reality: Anxiety often resurfaces once the chemical crutch is removed. Ongoing therapy is crucial.
Myth 2: "Only "hard" drugs cause addiction."
Reality: Even legal substances like caffeine or sugar can reinforce anxiety‑relief loops, especially when overused.
Myth 3: "I can quit on my own; I don’t need professional help."
Reality: The brain’s rewiring makes self‑detox dangerous for many substances. Medical supervision reduces relapse risk.

When to Seek Professional Help Right Away
If you notice any of the following, call a mental‑health or addiction specialist immediately:
- Thoughts of self‑harm or suicide.
- Severe withdrawal symptoms (e.g., seizures, hallucinations).
- Inability to function at work or school for more than a week.
- Legal trouble stemming from substance use.
Building a Personal Action Plan
Here’s a simple checklist you can print out and fill in daily:
- Identify your top three anxiety triggers.
- Note any substance you reach for after each trigger.
- Choose a healthier coping tool for each trigger (deep breathing, short walk, talking to a friend).
- Set a realistic reduction goal - e.g., cut alcohol from five drinks to three per week.
- Schedule at least one therapy or support session each week.
- Track progress in a journal; celebrate small wins.
Consistency beats perfection. Even a single day of healthier choices builds momentum.
Looking Ahead: Research Trends Shaping Future Treatment
Scientists are exploring psychedelics like psilocybin and MDMA as adjuncts to therapy for both anxiety and addiction. Early trials show promising reductions in cravings when paired with intensive counseling. While not mainstream yet, these studies hint at a future where we treat the mind and the habit loop together rather than in isolation.
Key Takeaways
- Anxiety often acts as a gateway to substance use because both target the brain’s reward system.
- Common coping substances include alcohol, opioids, benzodiazepines, and nicotine.
- Professional help-especially CBT and medication management-offers the highest success rates.
- Lifestyle habits (exercise, sleep, mindfulness) reinforce recovery.
- Early detection and a personalized action plan are essential to breaking the cycle.
Frequently Asked Questions
Can anxiety cause me to become addicted to prescription meds?
Yes. Many people with chronic anxiety are prescribed benzodiazepines or sleep aids. While these drugs can provide short‑term relief, they also carry a high risk of dependence if used regularly. A doctor can help taper the dose and introduce non‑addictive alternatives like SSRIs or therapy.
Is it possible to recover from both anxiety and addiction at the same time?
Absolutely. Integrated treatment programs address both conditions simultaneously, using a mix of counseling, medication, and peer support. Tackling them together avoids the “one‑or‑the‑other” trap that often leads to relapse.
What are the best non‑drug strategies for managing anxiety?
Regular exercise, mindfulness meditation, breathing exercises, and structured sleep routines are all evidence‑based. Pairing these with CBT or a support group maximizes their impact.
How long does it take to break the anxiety‑addiction cycle?
There’s no fixed timeline. Some people notice reduced cravings within weeks of therapy, while others may need months or longer. Consistency, professional guidance, and a supportive environment speed up recovery.
Are there any warning signs that my anxiety‑driven substance use is turning into an addiction?
Key signs include needing more of the substance to feel calm, feeling irritable when you can’t use it, hiding your usage, and letting it interfere with work or relationships. If any of these sound familiar, it’s time to seek help.

Tracy O'Keeffe
Honestly, the whole anxiety‑addiction link is just another buzzword circus, not a real crisis.
Rajesh Singh
We must recognize that self‑medicating with substances is a betrayal of one's moral duty to seek healthy coping. The article rightly points out the danger, but it also glosses over personal responsibility.
Albert Fernàndez Chacón
While personal responsibility matters, it's also vital to offer compassion; many people feel trapped by anxiety and need a non‑judgmental path to recovery.
Drew Waggoner
The piece paints a bleak picture, and for those already drowning, the weight of this information can feel crushing.
Mike Hamilton
Indeed, the interplay between stress hormones and reward circuits is a dance as old as humanity; understanding it invites us to rethink how we structure our societies.
Matthew Miller
Yo, this guide is a firestarter! Grab those coping tools and smash that anxiety‑addiction loop once and for all.
Liberty Moneybomb
But what if the real puppet masters are the pharma giants pushing us toward dependence, hiding behind “clinical care” while lining their pockets?
Alex Lineses
Let's focus on actionable steps: set small, measurable goals, lean on peer support, and keep a journal to track triggers and successes.
Brian Van Horne
To summarize, incremental progress coupled with professional guidance yields the highest probability of sustained remission.
Norman Adams
Oh great, another “holistic” cure-because adding more jargon surely resolves the deep‑rooted neurochemical mess.
Margaret pope
Remember each small win matters keep celebrating them and stay connected with supportive communities
Joe Moore
They don't tell you that the data in these articles is often skewed by funding from big pharma, making the whole narrative suspect.
Ayla Stewart
The emphasis on CBT and medication aligns with current best practices, showing a balanced approach to treatment.
Poornima Ganesan
The article does a decent job outlining the biochemical underpinnings of the anxiety‑addiction cycle, but it overlooks several critical nuances that any serious scholar would expect to see.
First, the role of genetic polymorphisms in dopamine transporter genes can predispose individuals to both heightened anxiety and substance craving, a factor rarely mentioned in popular health write‑ups.
Second, environmental stressors such as early childhood trauma interact with epigenetic mechanisms, effectively rewiring the hypothalamic‑pituitary‑adrenal axis.
Third, the discussion of benzodiazepine tapering fails to address the necessity of cross‑tapering strategies with alternative anxiolytics to prevent rebound hyper‑arousal.
Moreover, the claim that nicotine serves as a “calming” agent ignores the paradoxical increase in cortical excitability observed in chronic smokers.
In addition, the brief mention of psychedelics as future therapies is overly optimistic without acknowledging the stringent inclusion criteria of current clinical trials.
Furthermore, the article’s table could benefit from a more rigorous statistical representation, such as effect size metrics, rather than simplistic symptom listings.
It also neglects the socioeconomic determinants of health, which dramatically influence both access to treatment and relapse rates.
A comprehensive model must integrate behavioral economics to explain why individuals persist with maladaptive coping despite known long‑term costs.
From a therapeutic standpoint, incorporating acceptance and commitment therapy (ACT) alongside CBT can address experiential avoidance, a core component of anxiety‑driven substance use.
The absence of discussion on sleep hygiene protocols beyond generic advice is a missed opportunity, given the strong bidirectional link between insomnia and relapse.
Additionally, the article does not differentiate between short‑acting and long‑acting opioid formulations, which have distinct risk profiles.
Clinicians should also be vigilant about poly‑substance use patterns, as concurrent alcohol and opioid consumption exponentially raises overdose risk.
Lastly, patient education materials should be culturally tailored, recognizing that stigma varies across communities and can impede help‑seeking behavior.
In sum, while the piece provides a solid introduction, a deeper, interdisciplinary exposition would elevate it from a lay summary to an academically robust resource.
Emma Williams
Great points overall, looking forward to more detailed discussions