Think your scaly skin is just dry? Or that scratching makes it worse because you're doing something wrong? You're not alone. Millions of people see flaky, rough patches on their elbows, scalp, or knees and jump to conclusions-often the wrong ones. Scaly overgrowths of skin aren't one thing. They’re not always caused by poor hygiene, and they’re not always harmless. But the myths around them? Those are everywhere.
Myth: Scaly Skin Means You’re Not Hydrated Enough
Drink more water, they say. That’ll fix it. But if you’ve been chugging eight glasses a day and your skin still flakes like old paint, you’re not failing-you’re misinformed. While hydration matters, dry skin from low water intake rarely causes thick, scaly patches. Real scaly overgrowths like psoriasis or seborrheic dermatitis are immune-driven. They happen because your body makes skin cells too fast. These cells pile up before they can shed naturally. It’s not about how much you drink. It’s about how your immune system behaves.
A 2023 study in the Journal of the American Academy of Dermatology tracked 1,200 people with chronic scaling. Only 7% saw improvement after increasing water intake alone. The rest needed targeted treatments-topical steroids, retinoids, or light therapy. Drinking water helps your overall health. But it won’t dissolve a plaque of psoriasis.
Myth: Scratching Makes It Worse Because You’re Irritating It
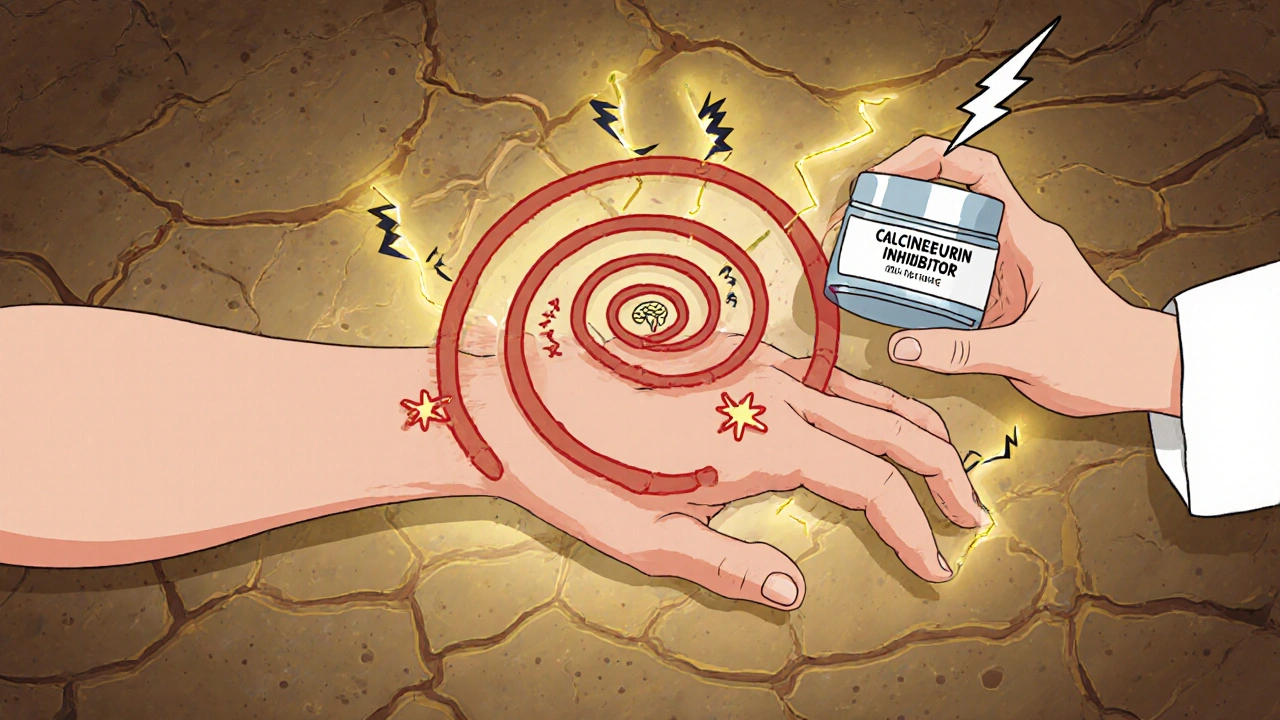
Yes, scratching feels bad. Yes, it can break the skin. But the real problem isn’t the scratching itself-it’s what’s underneath. When you have a scaly overgrowth like lichen planus or chronic eczema, your nerves are hypersensitive. The itch isn’t from dirt or irritation. It’s from inflammation signaling your brain: something’s wrong here.
Scratching gives temporary relief because it overloads those nerve signals. But it also triggers more inflammation. That’s why the itch-scratch cycle keeps going. It’s not a habit. It’s a biological loop. The solution isn’t just to stop scratching. It’s to break the inflammation cycle. Topical calcineurin inhibitors like tacrolimus or crisaborole reduce that signal at the source. Cold compresses, moisturizers with ceramides, and avoiding harsh soaps help too. But telling someone to just “stop scratching” is like telling someone with a migraine to just “stop feeling pain.”
Myth: All Scaly Skin Is Psoriasis
Psoriasis gets all the attention. Thick, red, silver-scaled plaques on elbows and knees? That’s the poster child. But not every flaky patch is psoriasis. Eczema (atopic dermatitis) often looks similar-dry, itchy, red-but the scales are finer, less defined, and usually show up in the creases of the skin. Fungal infections like tinea corporis (ringworm) can also flake and spread in circles. Seborrheic dermatitis flakes yellowish oil on the scalp, nose, and chest. Even skin cancer, like mycosis fungoides, can mimic scaling.
Here’s the difference: psoriasis scales are usually thick, well-demarcated, and bleed slightly when scraped (Auspitz sign). Eczema is more about cracks and oozing. Fungal scaling responds to antifungals within two weeks. Psoriasis? It doesn’t budge without immunomodulators.
Self-diagnosing based on internet images leads to wrong treatments. Using steroid cream on a fungal infection can make it worse. Using antifungal on psoriasis? Nothing happens. That’s why a dermatologist’s exam-even a quick one-is worth it. A Wood’s lamp, skin scraping, or biopsy can tell you what you’re really dealing with.
Myth: Natural Remedies Like Coconut Oil or Apple Cider Vinegar Cure Scaly Skin
Coco oil soothes. Vinegar stings. Both are popular online. But “natural” doesn’t mean “effective” or “safe.” Coconut oil can help moisturize mild dryness. But if you have psoriasis with thick plaques, it won’t penetrate. Apple cider vinegar? It’s acidic. Applying it to cracked, inflamed skin can burn. One patient in Brisbane reported chemical burns after using vinegar on scalp psoriasis. She ended up in the clinic with a secondary infection.
Some natural ingredients have limited support. Aloe vera may reduce redness slightly. Oatmeal baths can calm itch. But none of them alter the underlying immune response. If you’re using these as a replacement for proven treatments, you’re delaying real progress. That’s not holistic-it’s risky.
Think of it like this: if you had a broken bone, you wouldn’t just wrap it in a warm towel and hope it heals. You’d get an X-ray and a cast. Same with skin. Supportive care helps. But it doesn’t fix the root cause.
Myth: Scaly Skin Will Go Away If You Just Ignore It
Some people wait. They hope it fades. Maybe it does-for a while. But conditions like psoriasis, lichen simplex chronicus, or even early-stage cutaneous T-cell lymphoma don’t vanish on their own. They often get worse. Psoriasis plaques can expand. Eczema can thicken into leathery patches. Fungal infections spread to other body parts.
Ignoring it also increases the risk of infection. Broken skin from scratching is a doorway for bacteria. Staph infections are common in people with untreated eczema. In rare cases, chronic inflammation from unmanaged scaling can lead to joint damage (psoriatic arthritis) or affect mental health. Anxiety and depression are twice as common in people with visible skin conditions.
It’s not about being dramatic. It’s about catching it early. A mild case of seborrheic dermatitis treated with ketoconazole shampoo now can prevent years of dandruff, redness, and embarrassment. Waiting doesn’t make it go away. It makes it harder to treat.

Myth: Only Adults Get Scaly Skin Problems
Infants get cradle cap-that’s seborrheic dermatitis. Kids get eczema. Teens get scalp psoriasis. It’s not an aging thing. In fact, psoriasis often starts between ages 15 and 35. Eczema shows up in 20% of children under five. Many adults think their child’s flaky scalp is just “baby dryness.” It’s not. If it’s thick, yellow, or spreading, it needs attention.
Parents often delay seeing a doctor because they think it’s “just a phase.” But early intervention changes outcomes. Moisturizing routines, gentle cleansers, and low-dose topical treatments can prevent lifelong flare-ups. The same goes for teens. Scalp scaling that looks like dandruff might be psoriasis-and it responds better to early treatment.
What Actually Works
So what do you do when you see scaling? First, stop guessing. Look for these signs:
- Thick, silvery scales? → Likely psoriasis
- Red, cracked, itchy skin in folds? → Likely eczema
- Yellow, greasy flakes on scalp or eyebrows? → Likely seborrheic dermatitis
- Ring-shaped, expanding patches? → Likely fungal
- Scaling that won’t improve after 2 weeks of moisturizing? → See a doctor
For mild cases: use fragrance-free moisturizers daily. Apply them right after showering. Switch to gentle, soap-free cleansers. Avoid hot showers. Wear cotton clothes.
For moderate to severe: see a dermatologist. Treatments include topical corticosteroids, vitamin D analogs, calcineurin inhibitors, phototherapy, or oral medications like methotrexate or biologics. These aren’t “strong drugs.” They’re targeted tools. They work because they address the biology-not just the surface.
Final Thought: It’s Not About Perfection
You don’t need flawless skin. You need control. Scaly overgrowths are chronic. They come and go. But with the right approach, you can reduce flares, prevent complications, and live without shame. The biggest mistake? Believing the myths. The best move? Getting accurate info-and acting on it.
Is scaly skin always a sign of something serious?
Not always. Mild flaking from dry weather or harsh soaps is common and harmless. But if the scaling is thick, red, itchy, spreading, or doesn’t improve after two weeks of basic care, it could be psoriasis, eczema, a fungal infection, or another condition that needs medical attention.
Can stress cause scaly skin?
Stress doesn’t cause scaly skin, but it’s one of the top triggers for flare-ups in conditions like psoriasis and eczema. When you’re stressed, your body releases cortisol and other chemicals that ramp up inflammation. That’s why many people notice worsening skin during exams, job changes, or family crises. Managing stress through sleep, exercise, or mindfulness can help reduce flares.
Are scaly skin conditions contagious?
Most aren’t. Psoriasis, eczema, and lichen planus are immune-related, not infectious. The only common scaly condition that’s contagious is ringworm (tinea), which is caused by fungi. You can catch it from shared towels, gym equipment, or pets. If you’re unsure, avoid sharing personal items until you know the cause.
Why does my skin scale more in winter?
Cold air holds less moisture, and indoor heating dries out your skin even more. This worsens dryness and can trigger flare-ups in eczema and psoriasis. The lack of sunlight in winter also reduces vitamin D, which helps regulate skin cell growth. Using a humidifier, applying thicker moisturizers, and limiting hot showers can help.
Can diet cure scaly skin conditions?
No diet can cure psoriasis, eczema, or other scaly skin conditions. But some people notice improvements by reducing sugar, alcohol, or processed foods. Omega-3 fatty acids from fish or flaxseed may help reduce inflammation slightly. Still, dietary changes are supportive-not curative. Don’t replace medical treatment with a cleanse or elimination diet.

Andrea Johnston
So let me get this straight - you’re telling me my 3-year-old’s flaky scalp isn’t just ‘bad hair days’? I’ve been ignoring it because I thought it was dryness from shampoo. Now I’m terrified I’ve been letting psoriasis fester. Thanks for the wake-up call. I’m booking a dermatologist tomorrow.
Also - coconut oil? I’ve been slathering it on like it’s holy water. Guess I’m the human version of a greasy pancake now.
Scott Macfadyen
My cousin had this exact thing. Thought it was eczema. Used hydrocortisone for months. Turned out to be ringworm. The doctor laughed when he saw the Wood’s lamp results - glowing green like a alien tattoo. Don’t guess. Get it checked. Even if you think you’re being dramatic.
Also, stop reading Reddit dermatology threads. They’re all just people with 20 tabs open and zero medical licenses.
Denise Cauchon
OH MY GOD. I’ve been using apple cider vinegar on my scalp for 18 months because some ‘natural healer’ on Instagram said it’s a ‘miracle detox.’ I had a chemical burn last winter. My hair fell out in patches. I thought I was going bald from stress.
Turns out I had scalp psoriasis. And I treated it like I was trying to clean a dirty toilet. I’m crying. Not because I’m dramatic - because I’m furious at myself.
Also, why does everyone on the internet think ‘natural’ means ‘safe’? If it’s not FDA-approved, it’s a gamble with your skin. And I’m not paying for that lesson twice.
Premanka Goswami
They don’t want you to know the truth. The government, Big Pharma, and the dermatology cartel are all in cahoots. Why? Because if you knew scaly skin was just your body rejecting glyphosate from your cereal and tap water, you wouldn’t need $800 biologics.
My uncle in Punjab cured his psoriasis by drinking distilled moonshine and sleeping under a copper pyramid. He’s 89 and still walks barefoot on frozen tundra. They silenced him. They always silence the truth-tellers.
Wear aluminum foil hats. It blocks the EMF that triggers your immune system’s betrayal.
Alexis Paredes Gallego
Okay, but what if I told you… the real cause is 5G towers? No, seriously. Look at the correlation - psoriasis spikes in urban areas with dense cell networks. The skin is just your body’s way of screaming ‘I’m being microwaved!’
And don’t get me started on ‘vitamin D’ being the fix. They’re lying. The sun doesn’t heal - it’s the placebo effect of people thinking they’re ‘getting natural light.’ Meanwhile, the real cure? Quit eating gluten. Or maybe it’s the fluoride. Or both. I don’t know. But I know it’s not what they’re telling you.
Also, I’ve been using neem oil and it’s ‘working.’ Probably because I stopped trusting doctors. Coincidence? I think not.
Saket Sharma
Psoriasis = Th17/IL-23 axis dysregulation. Eczema = filaggrin mutation + barrier dysfunction. Fungal = dermatophyte invasion. Stop conflating pathophysiologies. Your ‘myth’ list is accurate, but your audience needs precision, not platitudes.
Topical calcineurin inhibitors = non-steroidal immunomodulators. Not ‘magic creams.’
Stop saying ‘see a dermatologist.’ Say: ‘get a biopsy if scaling persists beyond 14 days.’
Also, coconut oil is comedogenic. Don’t use it on inflamed skin. It’s basic dermatology. You’re not helping by being vague.
Shravan Jain
the truth is... nobody cares. you think your skin is special? it's not. everyone has flaky bits. you're just sensitive. and you're reading this because you're bored. or lonely. or both.
drinking water? useless. vinegar? burns. coconut oil? greasy mess. doctors? overpaid. biologics? expensive. and yet... you still click. why? because you want someone to say 'it's not your fault.'
it's not your fault. but it's also not a mystery. it's biology. and biology doesn't care about your feelings.
go outside. stop staring at your skin. live.
Brandon Lowi
Let me just say this - with the punctuation of a man who’s been screaming into the void for 17 years: What you’re seeing? It’s not a skin condition. It’s a cry for help from your immune system, screaming, ‘I AM TIRED OF BEING ATTACKED BY YOUR LIFESTYLE!’
You’re eating processed junk. You’re glued to screens. You’re sleeping like a zombie. You’re stressed out of your skull. And now your skin is paying the price - in scales, in cracks, in shame.
And yes - I know you’ve tried ‘moisturizers.’ But you’re treating the symptom like it’s the villain. The villain is your 3 a.m. snack of Cheetos and Netflix trauma.
Fix your sleep. Fix your stress. Fix your damn diet. The rest? It’s just the fallout.
And if you still have scaling after that? Then, yes - see a dermatologist. But don’t blame the skin. Blame the life that made it suffer.