Tramadol Seizure Risk Calculator
About This Tool
This tool assesses your individual risk of experiencing seizures while taking tramadol based on key risk factors discussed in the article. It's not a medical diagnosis but can help you identify whether you should discuss tramadol with your doctor.
Risk Assessment
Your Risk Assessment
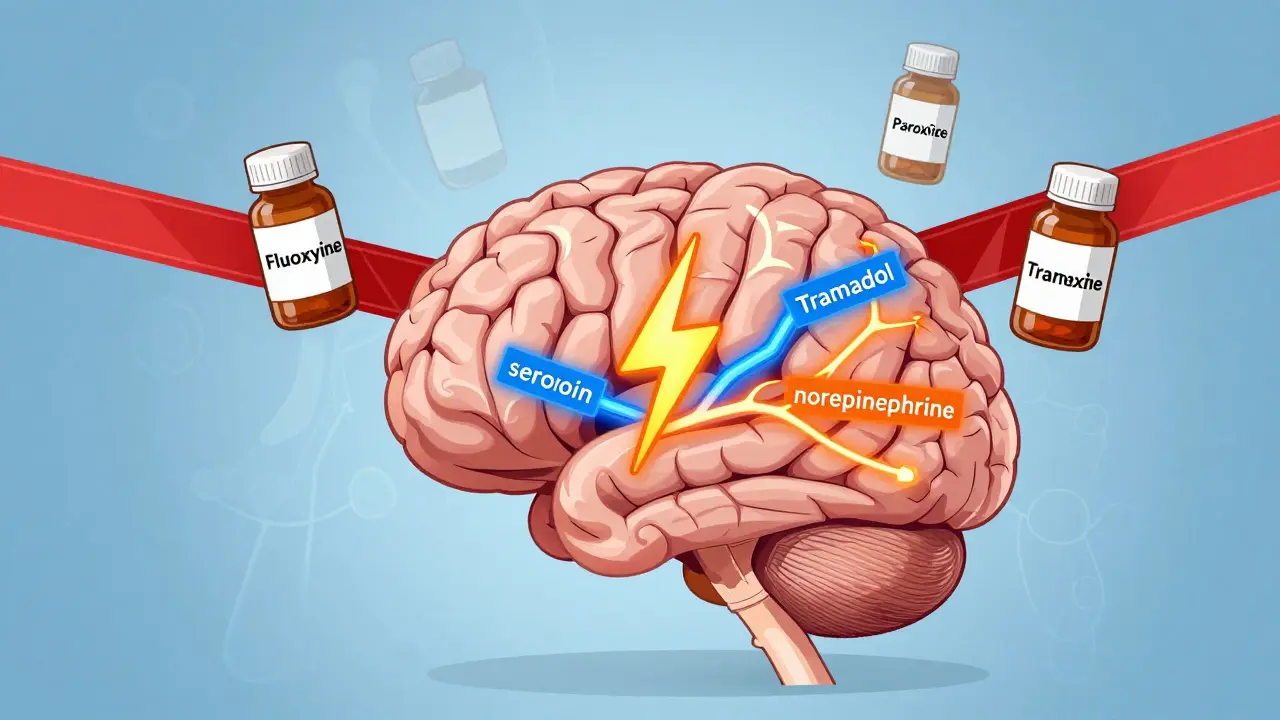
Tramadol is one of the most commonly prescribed pain medications in the U.S., with over 38 million prescriptions filled in 2022 alone. But for many people, this drug carries a hidden danger: seizures. Unlike other opioids, tramadol doesn’t just act on pain receptors - it also interferes with serotonin and norepinephrine in the brain. This dual action makes it effective for some types of chronic pain, but it also puts certain people at serious risk. The question isn’t just whether tramadol can cause seizures - it’s who is most likely to have them.
Who’s Most at Risk for Tramadol-Induced Seizures?
Not everyone who takes tramadol will have a seizure. But for some, the risk is far higher than most doctors realize. Research shows that seizure risk isn’t just about taking too much - it’s about your body, your other medications, and your medical history.
One of the clearest risk factors is a history of seizures or epilepsy. A 2019 study of 167 patients admitted to emergency rooms after tramadol overdose found that those with prior seizure disorders were over 3.7 times more likely to have a seizure from tramadol than those without. This isn’t a small increase - it’s a red flag. If you’ve ever had even one unexplained seizure in your life, tramadol could trigger another, even at normal doses.
Another major group at risk is older adults, especially those over 65. Their bodies process drugs slower. Kidney and liver function decline with age, and many take multiple medications. A 2023 study of over 70,000 nursing home residents found that those taking tramadol along with certain antidepressants had a 9% higher seizure rate than those on other painkillers. That might sound small, but in a population of tens of thousands, it means thousands of preventable seizures each year.
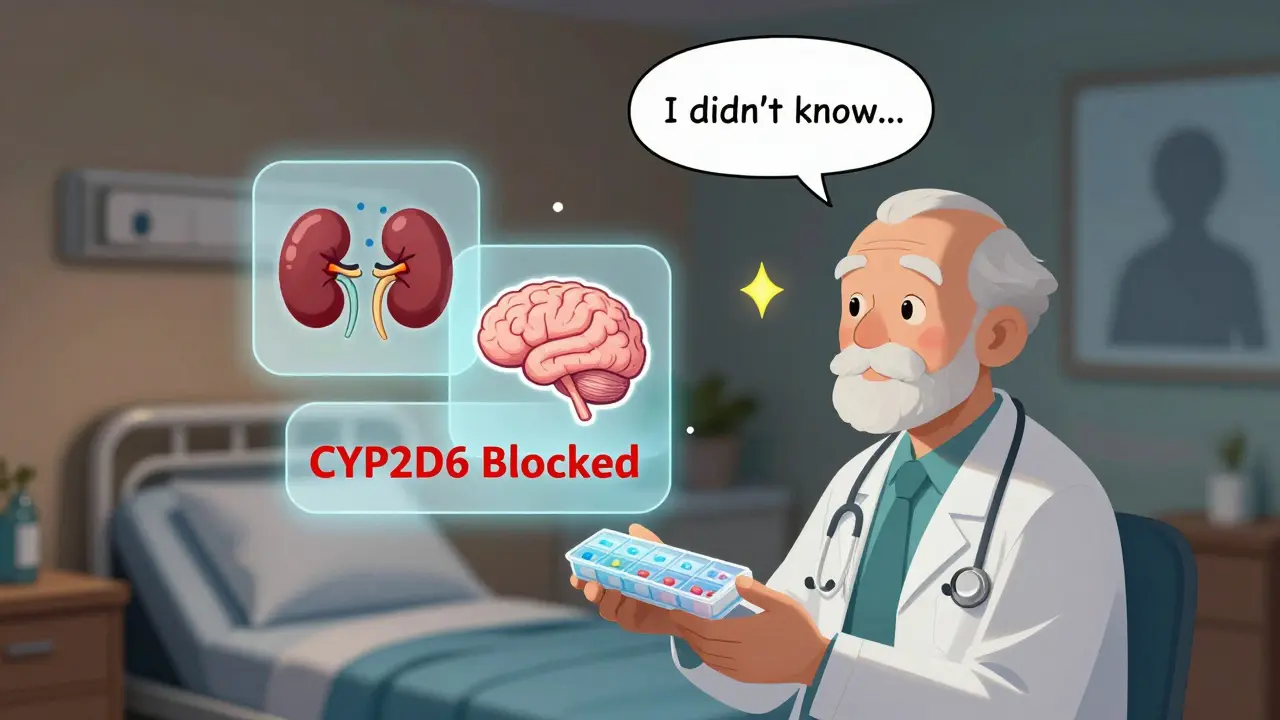
The Dangerous Interaction: CYP2D6 Inhibitors and Tramadol
Here’s where things get tricky - and why many patients are caught off guard. Tramadol needs to be broken down by an enzyme called CYP2D6 to work properly. But many common antidepressants block this enzyme. When that happens, two problems occur: the drug doesn’t work as well (leading patients to take more), and unmetabolized tramadol builds up in the body - which lowers the seizure threshold.
The worst offenders are:
- Fluoxetine (Prozac)
- Paroxetine (Paxil)
- Amitriptyline (Elavil)
- Sertraline (Zoloft) - though less potent, still risky in combination
A landmark study from The Ohio State University tracked 10 years of Medicare data and found that patients on tramadol plus one of these drugs had significantly more seizures than those on tramadol with safer alternatives like citalopram or escitalopram. Even more surprising: the risk didn’t depend on which drug was started first. Whether you were on the antidepressant for years and then started tramadol - or vice versa - the danger was still there.
What makes this interaction so dangerous is that doctors often don’t connect the dots. A patient with depression and chronic back pain might get prescribed both drugs without anyone realizing the risk. One Reddit user, ‘PainPatient87’, shared: “My neurologist didn’t mention the seizure risk when adding tramadol to my sertraline… I had my first seizure at 32 and now I’m on lifelong anti-epileptics.” This isn’t an outlier - it’s a pattern.
Dose Matters - But Not the Way You Think
You might assume that seizures only happen with overdoses. That’s not true. While higher doses definitely increase risk, seizures can occur even at prescribed levels. The 2011 study from Tehran found that patients taking doses as low as 300mg daily - well under the 400mg maximum - still had seizures.
What matters more than the total dose is how your body handles it. Some people are naturally slow metabolizers of CYP2D6. A 2023 study from the University of Toronto found that these individuals had 3.2 times higher tramadol levels in their blood than normal metabolizers - even when taking the same dose. That means two people on identical prescriptions can have wildly different outcomes.
Also, the timing of seizures is predictable. Most happen within 6 hours after taking the drug, with the average at 2.6 hours. If you’re on tramadol and feel unusual tingling, dizziness, or muscle twitching, don’t ignore it. These can be early signs.
Other High-Risk Groups
Beyond antidepressant interactions and seizure history, other factors raise risk:
- Renal impairment: If your kidneys don’t filter well (creatinine clearance below 60 mL/min), tramadol builds up. The FDA recommends reducing the daily dose to 300mg or less - and avoiding it entirely if clearance is below 30 mL/min.
- Alcohol or benzodiazepine use: Both lower the seizure threshold. Combining them with tramadol is dangerous.
- Head trauma or brain injury: Even years after the injury, the brain can be more sensitive to drug-induced seizures.
- Youth and recreational use: The 2019 emergency room study found 85% of tramadol-induced seizure patients were male, with a median age of 23. Many were using tramadol recreationally, sometimes in combination with stimulants or other painkillers.
What Should You Do?
If you’re taking tramadol, here’s what to ask your doctor:
- Do I have a history of seizures or epilepsy? If yes, tramadol is likely not safe.
- What antidepressants or other medications am I on? Tell them every pill, including over-the-counter ones like dextromethorphan (cough syrup).
- Have my kidneys been checked recently? A simple blood test can show if your creatinine clearance is low.
- Are there safer alternatives? Acetaminophen, NSAIDs (if appropriate), or non-opioid nerve pain drugs like gabapentin may be better choices.
For older adults, the American Geriatrics Society now lists tramadol as a potentially inappropriate medication due to seizure risk - especially when combined with serotonergic drugs. That doesn’t mean it’s never used, but it means it should be a last resort, not a first.
What’s Changing in Guidelines?
Regulators are catching up. The FDA updated tramadol’s label in January 2022 to lower the maximum daily dose for people with kidney issues. The European Medicines Agency added stronger seizure warnings in 2015. New Zealand’s drug safety agency flagged tramadol as the top cause of drug-induced seizures among prescription medications back in 2007 - and their warnings were spot on.
Now, research is moving toward personalized medicine. A blood test to check CYP2D6 metabolism status could soon become standard before prescribing tramadol. Until then, the safest approach is simple: know your risks, know your meds, and don’t assume your doctor knows them all.
Tramadol isn’t inherently evil. For some people, it works well and safely. But for others - especially those with depression, kidney trouble, or a history of seizures - it’s a ticking time bomb. The key is not avoiding pain treatment. It’s choosing the right one.
Can tramadol cause seizures even at prescribed doses?
Yes. Seizures can occur at standard therapeutic doses, especially in people with risk factors like epilepsy, kidney problems, or when taken with certain antidepressants. Studies show seizures happen even below the 400mg daily limit, particularly in slow metabolizers of the CYP2D6 enzyme.
Which antidepressants increase seizure risk with tramadol?
Antidepressants that inhibit the CYP2D6 enzyme significantly raise seizure risk when taken with tramadol. These include fluoxetine (Prozac), paroxetine (Paxil), amitriptyline (Elavil), and to a lesser extent, sertraline (Zoloft). Safer alternatives include citalopram and escitalopram, which do not block this enzyme.
Is tramadol safe for older adults?
The American Geriatrics Society advises against using tramadol in older adults due to increased seizure risk, especially when combined with other medications. Kidney function declines with age, slowing drug clearance. The FDA recommends a maximum daily dose of 300mg for those with reduced kidney function, and many experts suggest avoiding tramadol entirely in favor of safer pain relievers like acetaminophen.
How soon after taking tramadol can a seizure occur?
Most tramadol-induced seizures occur within 6 hours of ingestion, with the average time being 2.6 hours. This tight window makes it easier to identify the cause if a seizure happens shortly after taking the drug. Monitoring for symptoms like dizziness, muscle stiffness, or unusual sensations during this time is critical.
Should I stop tramadol if I’m on an antidepressant?
Don’t stop suddenly - that can cause withdrawal or worsen pain. Talk to your doctor. If you’re taking a CYP2D6-inhibiting antidepressant like fluoxetine or paroxetine, ask if switching to a non-inhibiting option like citalopram is possible. If not, consider alternative pain treatments. Never adjust doses on your own.
Are there tests to find out if I’m at higher risk?
Yes. A CYP2D6 genetic test can determine if you’re a poor, intermediate, extensive, or ultra-rapid metabolizer. Poor metabolizers are at highest risk because they build up more unmetabolized tramadol. While not yet routine, this test is becoming more available and may soon be recommended before starting tramadol, especially in patients on multiple medications.
Tramadol can be helpful - but only if used with full awareness of the risks. If you’re taking it, know your meds. Know your body. And never assume silence from your doctor means safety.
Alex Ogle
Man, I read this whole thing and I just sat there thinking about my uncle who took tramadol for his back pain after his surgery. He was on sertraline for anxiety, never said a word about the interaction. One night, he had this weird twitching, thought it was just nerves. Next thing you know, he’s in the ER with a seizure. They didn’t even connect it until his neurologist pulled up his med list. Scary stuff. I didn’t even know tramadol worked like that - I always thought it was just a weak opioid. Turns out it’s a chemical cocktail with a fuse.
And the worst part? He’s 71. Kidney function’s been declining for years. No one ever tested his CYP2D6. They just wrote the script like it was Tylenol. I’m telling you - this isn’t some edge-case risk. It’s a silent epidemic hiding in plain sight, in every primary care office in America.
Doctors get paid to write prescriptions. They don’t get paid to do pharmacokinetic deep dives. So we, the patients, have to be the watchdogs. Read the damn leaflets. Ask about alternatives. Don’t let ‘it’s been fine for years’ be your excuse. My uncle’s on gabapentin now. No more seizures. But he almost died because no one bothered to connect the dots.
Andy Cortez
so like… tramadol causes seizures?? wow. who knew. i mean, i thought it was just like vicodin but with extra serotonin?? lol. my cousin took it for a sprained ankle and ended up in a psych ward for 3 days. they said ‘it was probably the tramadol’ but the docs were like ‘huh, weird’ and moved on. like, seriously?? we’re still letting this stuff be prescribed like it’s a vitamin??
and dont even get me started on the ‘switch to citalopram’ advice. citalopram is basically liquid sadness. i’d rather have a seizure than feel like a zombie for 6 months. also, why is everyone so scared of the word ‘opioid’? it’s just a painkiller. we’re not trying to kill ourselves here. #stopovermedicating
Andrew Jackson
It is both a tragedy and a national disgrace that the American medical establishment has allowed this pharmaceutical negligence to persist. The FDA, in its bureaucratic inertia, has failed to enforce adequate safeguards for vulnerable populations - particularly the elderly, whose very physiology is being exploited by profit-driven pharmaceutical manufacturers. We are not a nation of rational thinkers; we are a nation of pill-popping automatons, obedient to the prescriptions of doctors who have been subtly coerced by pharmaceutical marketing.
Compare this to Germany, where CYP2D6 testing is routine before opioid administration. Or Japan, where tramadol is classified as a controlled substance with strict monitoring. Yet here, in the land of the free, we treat life-altering neurochemical interactions like a game of Russian roulette. Shameful. Un-American. And entirely preventable.
Joseph Charles Colin
Let me clarify a few misconceptions here. Tramadol’s seizure risk is not simply additive - it’s multiplicative. The CYP2D6 enzyme polymorphism creates a bimodal distribution: poor metabolizers (PMs) have 3-4x higher plasma concentrations of the parent compound, which directly lowers the GABAergic seizure threshold. Simultaneously, the nortramadol metabolite (M1), which is mu-opioid active, is reduced in PMs, diminishing analgesia - leading to dose escalation, which compounds the risk.
Furthermore, SSRIs like fluoxetine and paroxetine are potent CYP2D6 inhibitors with long half-lives (up to 16 days for fluoxetine). Even after discontinuation, inhibition persists. The 9% increase in seizure incidence among nursing home residents isn’t noise - it’s a population-level signal. The FDA’s 2022 dose reduction for renal impairment (300mg max) is a step, but it’s reactive, not proactive. We need preemptive genotyping, not post-seizure damage control.
Bottom line: If you’re on tramadol + an SSRI, and you’re over 60 or have eGFR <60, you’re in a high-risk cohort. The data is robust. The guidelines are clear. Ignorance isn’t a defense - it’s a liability.
John Sonnenberg
I’ve been on tramadol for 8 years. 400mg daily. No seizures. No issues. No problems. My doctor says I’m an extensive metabolizer. I got tested. I’m fine. So why are you all acting like everyone’s going to have a seizure? You’re scaring people with cherry-picked stats. My cousin had a seizure once when she was 19 and drunk. That’s not tramadol. That’s alcohol. And now she’s convinced she’s epileptic. Stop the fearmongering.
Also, why is everyone obsessed with CYP2D6? It’s one enzyme. I’ve been on Prozac for 12 years. I took tramadol for a year. Nothing. Not even a headache. Maybe your body is different. Maybe you’re just weak. Or maybe you’re just looking for drama.
Joshua Smith
This is super helpful. I’ve been on tramadol for my fibromyalgia and sertraline for anxiety for about three years. I never knew they could interact like this. I’ve had some weird muscle twitches after taking it, especially in the first hour - thought it was just stress. But now I get it. I’m going to ask my doctor about switching to escitalopram. Also, I didn’t even know about the CYP2D6 test. That sounds like something I should get done. Thanks for laying this out so clearly. I feel less scared now that I understand what’s going on.
Jessica Klaar
I’m a nurse in a geriatric unit, and I’ve seen this happen too many times. An elderly patient on tramadol and paroxetine - both prescribed by different specialists. No one talked to each other. One morning, Mrs. Thompson had a tonic-clonic seizure in the hallway. We rushed her in. Her family was devastated. She’d been fine for months. Then we checked her labs - creatinine clearance was 42. She was on 300mg daily. The dose should’ve been cut to 100mg. She didn’t even know what CYP2D6 was. No one explained it. We lost three weeks of her life to the hospital, and she’ll never walk without a cane again.
This isn’t just about science. It’s about communication. And compassion. We need better handoffs between specialists. We need patient education that doesn’t read like a textbook. And we need to stop assuming that ‘no complaints’ means ‘no risk.’
PAUL MCQUEEN
Wow. So you’re saying we should stop using tramadol entirely? That’s just… lazy medicine. If people can’t handle a little risk, maybe they shouldn’t be in pain. I mean, look - there are worse things than seizures. Like not being able to work. Or not being able to hold your grandkids. You want to live in a world where every drug has a 0% risk? That’s not medicine. That’s fantasy. And now we’re going to start genetic testing everyone before giving them pain relief? Next you’ll be asking for a background check on their liver.