When your doctor suggests switching from Humira to a biosimilar, it’s normal to feel uneasy. You’ve been stable on your medication for years. You know how your body reacts. So why change? And what exactly is a biosimilar anyway? These questions aren’t rare-they’re common. Despite billions in potential savings and FDA approval of 74 biosimilars as of April 2025, less than 10% of patients on eligible biologics actually switch. The reason? Fear, confusion, and misinformation.
What Biosimilars Really Are (And What They’re Not)
Biosimilars aren’t generics. That’s the first thing patients need to understand. Generics are exact chemical copies of small-molecule drugs like aspirin or metformin. They’re made in labs using predictable formulas. Biosimilars are different. They’re made from living cells-like yeast or hamster ovary cells-and are designed to be highly similar to complex biologic drugs like Enbrel, Remicade, or Herceptin. These biologics are proteins, often huge molecules with intricate 3D shapes that affect how they work in the body. The FDA doesn’t require biosimilars to be identical. They require no clinically meaningful differences in safety, purity, or potency. That means: if you respond well to the original drug, you’ll respond the same way to the biosimilar. Studies show this across conditions like rheumatoid arthritis, Crohn’s disease, and cancer. A 2024 meta-analysis of over 12,000 patients found no increase in adverse events or reduced effectiveness with biosimilars compared to their reference products. But here’s the catch: because biosimilars come from living systems, tiny variations can occur between batches. That’s why manufacturers must run over 100 analytical tests, plus animal studies and at least one small clinical trial to prove similarity. It’s a process that takes 8-10 years and costs $100-250 million. Compare that to generics, which take 3-4 years and cost $2-3 million. That’s why biosimilars aren’t cheap to make-but they’re still much cheaper than the original biologics.Why Patients Are Hesitant (And Why It’s Not Just About Price)
Most patients aren’t afraid of saving money. They’re afraid of something going wrong. A 2025 survey by the Evernorth Research Institute found that 79% of patients worry biosimilars won’t work as well. 63% fear new or different side effects. And 31% have never even heard of biosimilars-even though they’re already on a biologic. One Reddit user, ChronicPainPatient87, shared a story that echoes across patient forums: "My doctor switched me to a biosimilar without telling me. I had a flare-up. Now I’m terrified to switch again." That’s not just a bad experience-it’s a broken communication. When patients aren’t involved in the decision, trust evaporates. Even if the switch was medically sound, the lack of transparency made the patient feel like a test subject. Another hidden issue: cost savings aren’t reaching patients. While biosimilars cut system-wide costs by an estimated 35%, out-of-pocket prices often stay the same. For infliximab and pegfilgrastim, studies show patients still pay the same copay whether they get the brand or the biosimilar. Why? Pharmacy benefit managers (PBMs) and insurers sometimes structure rebates to favor the original drug-even when the biosimilar is cheaper. So patients don’t feel the benefit, even when the system does.Doctors Are Hesitant Too-And That Makes It Worse
Patients aren’t the only ones unsure. A 2025 report from the Center for Biosimilars found that only 68-88% of healthcare providers fully understood biosimilar safety and efficacy. Some doctors avoid recommending them because they’re unfamiliar. Others worry about administrative headaches: prior authorizations, formulary restrictions, or being blamed if a patient has a reaction. The FDA’s Dr. James Wilson made it clear in 2024: "All biosimilars in the U.S. should be interchangeable." Interchangeable means a pharmacist can swap the brand for the biosimilar without asking the doctor. Right now, only a handful of biosimilars have that status. But the FDA is moving toward it-and it’s a game-changer. When patients know their pharmacist can switch them without extra steps, trust grows.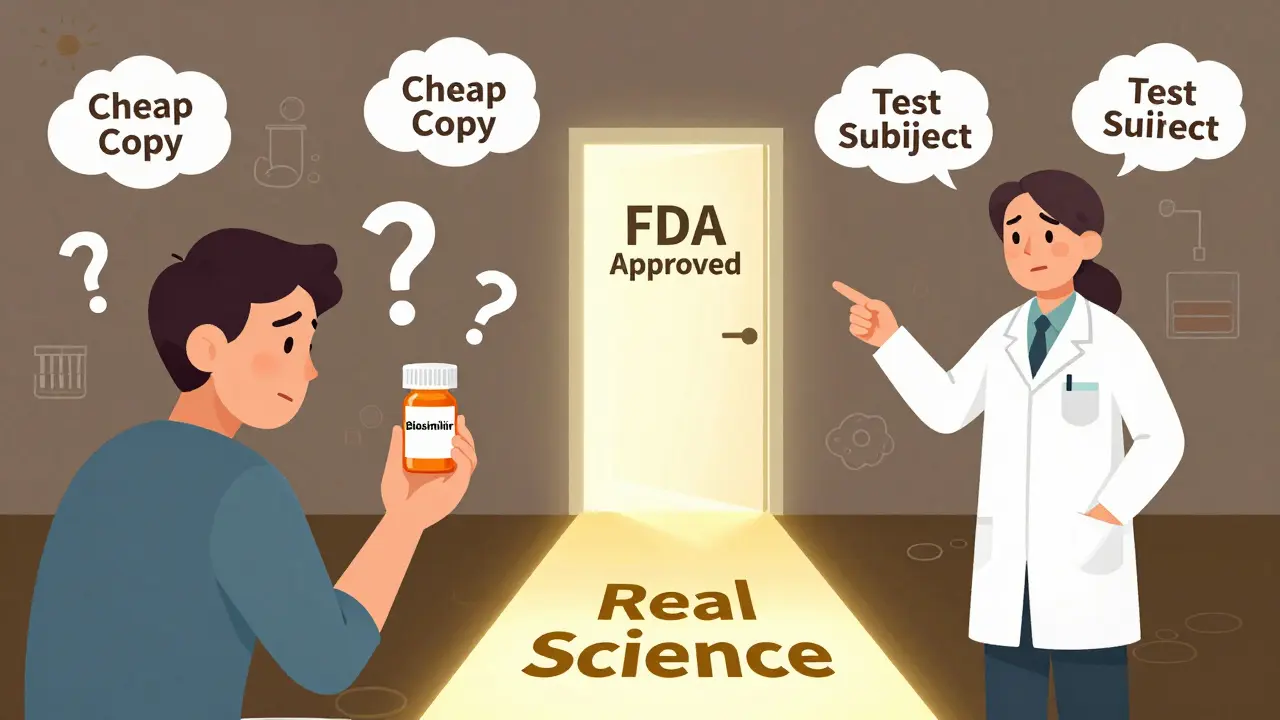
How to Build Trust: Real Talk, Not Brochures
You can’t fix hesitation with a pamphlet. You need real conversations. Here’s what works:- Use plain language. Don’t say "biosimilar." Say: "This is a version of your current drug, made in a similar way, tested just as thoroughly, and proven to work the same. It’s not a cheaper copy-it’s a scientifically approved alternative."
- Include patients in the decision. Ask: "Would you be open to trying this option? I can explain how it’s been tested, and we can monitor how you feel." That simple shift from directive to collaborative reduces anxiety.
- Share real-world data. Tell patients: "Over 10,000 people with rheumatoid arthritis have switched to this biosimilar. Their disease activity scores, lab results, and quality of life stayed the same as before."
- Track outcomes together. Use simple biomarkers-like CRP or ESR blood tests-to show improvement or stability after the switch. Seeing proof on paper helps silence doubts.
What’s Changing in 2025 and Beyond
The tide is turning. In April 2024, CVS removed Humira from most commercial formularies. ESI and OptumRx followed in 2025. That forced prescribers and patients to consider biosimilars. The result? A 2.3 percentage point drop in the average cost of biologics by August 2024. But patient satisfaction dropped too-by 15%. That’s a warning sign. Cost savings mean nothing if patients feel abandoned. The FDA’s 2024 draft guidance could speed things up. By letting manufacturers rely more on lab tests and less on new clinical trials, approval times could shrink. That means more biosimilars will hit the market. By 2034, nearly $232 billion in biologic sales will lose patent protection. If we get this right, biosimilars could save $300 billion between now and 2030. The biggest barrier isn’t science. It’s perception. Patients aren’t resisting innovation. They’re resisting being treated like a cost center.
What You Can Do Right Now
If you’re a patient:- Ask: "Is there a biosimilar version of my drug?"
- Ask: "Has this been tested on people like me?"
- Ask: "Will I pay less out of pocket?"
- Ask: "Can we track my symptoms and blood work after the switch?"
- Don’t assume patients know what biosimilars are. Explain them clearly.
- Don’t switch without consent. Even if it’s allowed, make it a shared decision.
- Document the conversation. Write down the patient’s concerns and how you addressed them.
- Use real data-not marketing materials-to support your recommendation.
Bottom Line: It’s Not About Cost. It’s About Care.
Biosimilars aren’t a trick. They’re not a compromise. They’re a scientifically validated option that can make life-changing treatments more accessible. But they won’t succeed if patients feel like they’re being swapped out for cheaper alternatives. The future of biosimilars doesn’t depend on more approvals or lower prices. It depends on trust. And trust is built one honest conversation at a time.Are biosimilars safe?
Yes. Every biosimilar approved by the FDA has undergone rigorous testing to prove it works the same as the original biologic drug. Studies involving tens of thousands of patients show no increase in side effects or loss of effectiveness. The FDA requires biosimilars to have no clinically meaningful differences in safety, purity, or potency.
How are biosimilars different from generics?
Generics are exact chemical copies of simple drugs like ibuprofen. Biosimilars are highly similar versions of complex biologic drugs made from living cells. Because biologics are large, intricate proteins, biosimilars can’t be identical-but they must prove they work the same way. This requires far more testing than generics.
Will I save money if I switch to a biosimilar?
Sometimes, but not always. While biosimilars reduce overall healthcare costs by about 35%, many patients still pay the same copay as they did for the brand-name drug. This is often because insurance plans and pharmacy benefit managers structure rebates to favor the original product. Ask your pharmacist or insurer: "Will my out-of-pocket cost go down?"
Can my pharmacist switch me to a biosimilar without asking my doctor?
Only if the biosimilar has been designated as "interchangeable" by the FDA. Right now, only a few have that status. Most require a new prescription from your doctor. But the FDA is moving toward making more biosimilars interchangeable, which will make switching easier and more automatic.
I had a flare-up after switching. Does that mean the biosimilar didn’t work?
Not necessarily. Flare-ups can happen for many reasons-stress, infection, diet, or even changes in your body’s response over time. A single flare doesn’t prove the biosimilar failed. But it does mean you should talk to your doctor. They can check your biomarkers (like CRP or anti-drug antibodies) and decide whether to stay on the biosimilar or switch back. Never assume the drug is the cause without testing.
Why aren’t there more biosimilars on the market?
Developing a biosimilar is expensive and complex-it can cost $100-250 million and take over 8 years. Some drugmakers also use legal and financial tactics to delay competition, like "pay-for-delay" deals. Plus, only 21% of patients know what biosimilars are, so manufacturers are cautious about investing without clear demand. But with nearly $232 billion in biologic sales set to lose exclusivity by 2034, more are coming.

Robert Way
so i switched to the biosimilar and my knees started actin up again like crazy
doc said it was fine but i swear i felt it in my bones the second they gave me the new bottle
now im scared to even look at a prescription
Sarah Triphahn
let me be real for a second - this whole biosimilar thing is just corporate greed dressed up as science
you think the FDA really cares about your health or are they just clearing the way for Big Pharma to keep raking in cash while pretending to save you money
remember when they said aspartame was safe? now we know better
same playbook. same lies. different drug name
you want to know why patients are hesitant? because we’ve been lied to too many times
they don’t want us to be healthy - they want us to be profitable
Jason Yan
hey i get why people are nervous - switching meds is scary, especially when you’ve been stable for years
but here’s what i learned after switching from Humira to a biosimilar for my psoriatic arthritis: nothing changed
same energy, same flare-ups (which were zero), same sleep, same life
the only difference? my insurance paid $300 less per month and i didn’t have to beg for prior auth every time
the science is solid - over 10k patients studied, FDA says no meaningful difference, real-world data backs it
it’s not about trusting the system - it’s about trusting the data
and if you’re worried about side effects? track your labs. CRP, ESR, your symptoms - write it down
if something changes, you’ll see it. if nothing changes? you just saved yourself hundreds and kept your life intact
trust isn’t built by forcing people - it’s built by giving them facts, space, and time
shiv singh
how dare they push this on us like we’re lab rats
they don’t care about us - they care about profits
my cousin got switched and now she’s on disability
no one asked her
no one told her
now she can’t even hold her baby
this isn’t medicine - this is murder by bureaucracy
someone needs to go to jail for this
Sarah -Jane Vincent
you all are being manipulated
the FDA doesn’t approve biosimilars - they rubber stamp them
did you know the same company that makes Humira also owns the biosimilar? same factory. same people. same vial
they just changed the label and called it a new drug
the ‘testing’? they reused the original clinical data
you think that’s safe? think again
this is how they control the market - make you think you have choice when you don’t
ask your pharmacist: who owns the biosimilar? you’ll be shocked
Henry Sy
bro i switched and my body went full nuclear
three days in - fever, rash, felt like i got hit by a truck made of disappointment
doc said it was ‘coincidental’
coincidental? my body didn’t do this for 5 years on Humira
now i’m back on the brand and i pay $1200 a month like a sucker
but at least i’m not dying
they don’t want you to know this - but the biosimilar market is a casino and we’re the chips
Alvin Bregman
look i used to be scared too
but after talking to my rheumatologist and reading the actual studies
i realized the fear was coming from not knowing
not the drug
they showed me the data
same results
same safety
same everything
now i save 70% and my insurance is happy
and i’m still alive
and my joints still work
maybe the problem isn’t the biosimilar
maybe its the silence around it
Anna Hunger
It is imperative to underscore that the regulatory framework governing biosimilar approval is among the most rigorous in pharmaceutical science.
The FDA mandates comparative analytical characterization, pharmacokinetic and pharmacodynamic studies, immunogenicity assessments, and clinical trials to demonstrate no clinically meaningful differences.
These are not merely ‘similar’ products - they are scientifically validated therapeutics with identical clinical outcomes in controlled and real-world settings.
Patients who express concern are not irrational; they are responding to a systemic failure in communication.
The responsibility lies with clinicians and institutions to provide transparent, evidence-based dialogue - not marketing pamphlets or rushed decisions.
Trust is not a marketing campaign. It is a clinical covenant.
Vicky Zhang
oh my gosh i just want to cry
i switched to the biosimilar and i thought i was gonna die
my hands were shaking, i couldn’t sleep, i felt like i was falling apart
but then i talked to my nurse and she said let’s check your CRP
it was lower than it had been in three years
i didn’t feel better - but my body was healing
and then i realized: i was scared of the change, not the drug
my fear was louder than my pain
and now? i’m on it for good
and i’m not afraid anymore
it’s not magic
it’s science
and it worked
Allison Deming
It is deeply concerning that the narrative surrounding biosimilars has been co-opted by fearmongering and misinformation, often propagated by individuals with no medical training.
The data is unequivocal: biosimilars are safe, effective, and equivalent to their reference biologics.
The fact that out-of-pocket costs remain unchanged is a failure of insurance policy design - not a reflection of the drug’s efficacy.
Patients must be empowered, not manipulated.
Providers must lead with transparency, not convenience.
And regulators must continue to enforce the highest standards - which they are.
Blaming biosimilars for systemic failures is not only inaccurate - it is dangerous.
Susie Deer
USA makes the best drugs
why are we letting foreign companies make our medicine
humira is american
biosimilar is made in china
you think they care about your life
they care about profit
stop giving away our health