Antacid Safety Checker for Kidney Disease
Is Your Antacid Use Safe?
This tool helps you determine if your antacid use is safe based on your kidney function stage and medication regimen. Always consult your nephrologist before making changes to your treatment.
Many people reach for antacids like Tums or Milk of Magnesia when they feel heartburn. It’s simple, cheap, and available on any pharmacy shelf. But if you have kidney disease, taking these over-the-counter meds without knowing the risks can be dangerous-sometimes life-threatening. The problem isn’t just heartburn. It’s what those antacids do to your body when your kidneys can’t keep up.
Why Antacids Are Used in Kidney Disease
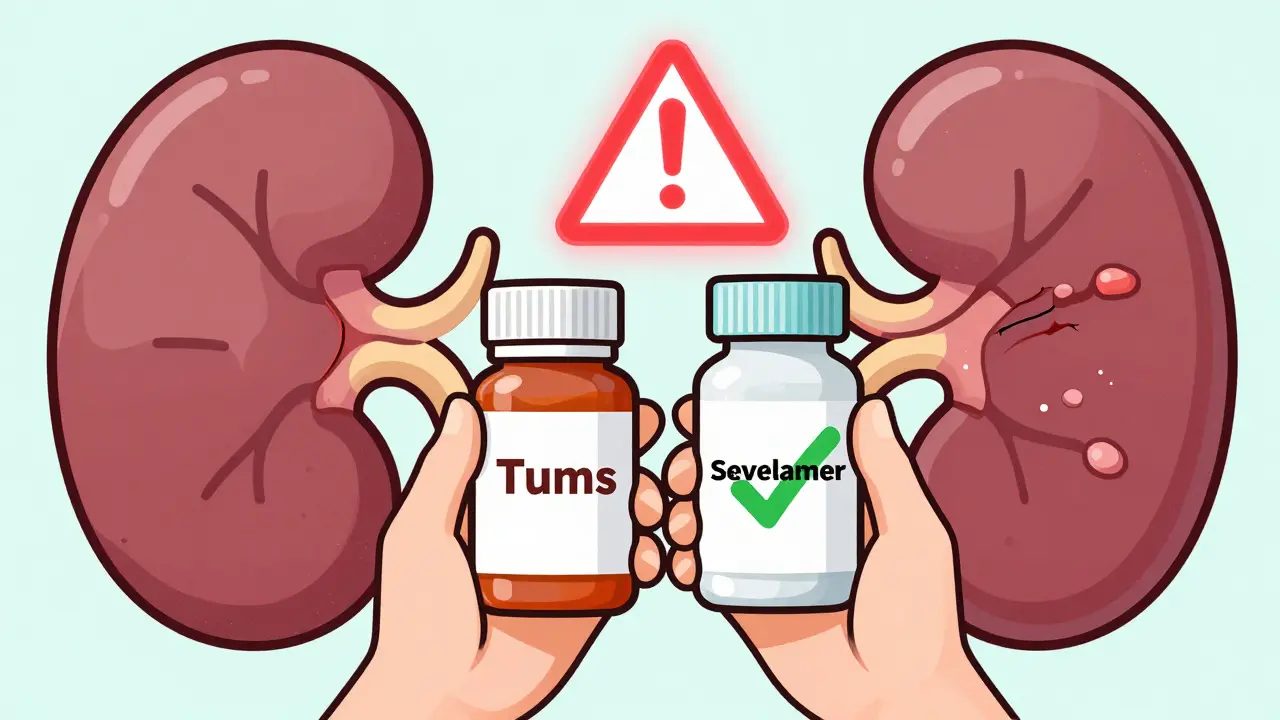
When your kidneys start to fail, they lose the ability to remove phosphate from your blood. Too much phosphate leads to weak bones, itchy skin, and dangerous calcification in your heart and blood vessels. That’s where antacids come in-not as heartburn remedies, but as phosphate binders. Calcium carbonate (Tums) and aluminum hydroxide work by sticking to phosphate in your food before it gets absorbed. They form a compound your body can’t absorb, so it passes out in your stool. For patients with early-stage kidney disease (stage 3), calcium-based antacids can be an affordable way to control phosphate levels. A single bottle of generic calcium carbonate costs about $10 a month. Compare that to prescription binders like sevelamer or lanthanum carbonate, which can run over $2,000 monthly. For many, especially without good insurance, antacids are the only option.The Hidden Dangers: Aluminum, Calcium, and Magnesium
But here’s the catch: your kidneys aren’t just filtering phosphate. They’re also in charge of balancing minerals like calcium, magnesium, and aluminum. When kidney function drops below 30% (GFR under 30 mL/min), these minerals start to build up-and that’s where things go wrong. Aluminum is the most dangerous. Even small amounts can stick to your bones and brain. Long-term use of aluminum-containing antacids can cause dialysis dementia, bone pain, and anemia. The FDA has warned since 1990 that these products should never be used for more than two weeks in people with normal kidneys. For someone with advanced kidney disease, even a few doses can be risky. Most nephrologists avoid aluminum binders entirely unless it’s a last-resort emergency. Calcium seems safer, but it’s not. Too much calcium in the blood leads to calcification-hard deposits in your arteries and heart valves. Studies show CKD patients with calcium levels above 10.2 mg/dL have a 30-50% higher risk of heart attack or stroke. One patient in Brisbane shared that after taking Tums daily for six months, his calcium hit 11.2 mg/dL. A CT scan showed new calcification in his coronary arteries. He didn’t know antacids could do that. Magnesium is another silent killer. Milk of Magnesia is popular for constipation, but in kidney disease, magnesium builds up fast. At levels above 4 mg/dL, you get muscle weakness. At 8 mg/dL, you can lose control of your legs. Above 10 mg/dL, your breathing slows. Above 15 mg/dL, it can stop your heart. There are documented cases of dialysis patients ending up in the ER after using over-the-counter magnesium products for constipation.Prescription Binders vs. Antacids: What’s the Difference?
Prescription phosphate binders were designed for kidney patients. They’re more precise, safer, and don’t carry the same risks.- Sevelamer (Renagel): Non-calcium, non-aluminum. Reduces phosphate by 25-35% per meal. No risk of hypercalcemia. Costs about $2,000-$2,500/month.
- Lanthanum carbonate (Fosrenol): Also non-calcium. Similar effectiveness to sevelamer. Higher pill burden. Around $2,500-$3,500/month.
- Sucroferric oxyhydroxide (Velphoro): Iron-based. Fewer pills per dose. Costs $4,000/month.

Who Should Use Antacids-and Who Should Avoid Them
It’s not black and white. But there are clear guidelines from KDIGO and the National Kidney Foundation:- CKD Stage 3 (GFR 30-59): Calcium carbonate may be used under supervision. Dose: 600-1200 mg elemental calcium per meal. Monitor calcium monthly. Avoid magnesium and aluminum completely.
- CKD Stage 4-5 (GFR under 30): Avoid all antacids as phosphate binders. Use only prescription binders. If you need heartburn relief, calcium carbonate may be used occasionally-but only if taken at least two hours before or after your phosphate binder. Never take it daily.
- Dialysis patients: Absolutely avoid aluminum and magnesium antacids. Calcium antacids require extreme caution. Even one extra tablet can push calcium into the danger zone.
Drug Interactions You Can’t Afford to Ignore
Antacids don’t just affect phosphate. They mess with how your body absorbs other medications. If you’re on blood pressure pills, antibiotics, thyroid meds, or seizure drugs, antacids can make them useless.- Phenytoin (for seizures): Antacids can reduce absorption by up to 40%.
- Levothyroxine (for thyroid): Take it at least four hours before or after any antacid.
- Antibiotics like ciprofloxacin or tetracycline: Antacids block absorption completely.
What Patients Are Saying
On patient forums, stories are heartbreaking. One woman in Ohio took Milk of Magnesia for constipation for weeks. Her magnesium level hit 8.7. She couldn’t walk. She spent five days in the hospital. Another man in Texas used Tums daily for heartburn. His nephrologist found his calcium was sky-high. He needed surgery to remove calcified arteries. A 2022 survey by the American Association of Kidney Patients found that 68% of CKD patients couldn’t tell the difference between a prescription phosphate binder and an over-the-counter antacid. Nearly half had used antacids without telling their doctor. That’s not ignorance-it’s a system failure. Doctors don’t always warn patients. Pharmacists don’t always ask about kidney disease. Patients assume all antacids are the same.
What You Should Do
If you have kidney disease:- Don’t take any antacid without talking to your nephrologist. Even if it’s just for heartburn.
- Know your numbers. Ask for your latest serum calcium, phosphate, magnesium, and aluminum levels. Know what’s normal for you.
- Read labels. Look for “calcium carbonate,” “aluminum hydroxide,” or “magnesium hydroxide.” If you see them, ask your doctor if it’s safe.
- Never use antacids daily as phosphate control unless approved. Prescription binders exist for a reason.
- Report symptoms. Nausea, confusion, muscle weakness, or irregular heartbeat? Call your doctor. It could be mineral toxicity.
What’s Changing Now
The FDA issued new warnings in March 2023 requiring stronger labels on aluminum antacids for kidney patients. Medicare now tracks hospitalizations from antacid misuse in CKD patients as a quality metric. The NIH just launched a $12.5 million study tracking 5,000 patients to create better guidelines. New drugs like tenapanor (Xphozah) are coming. Instead of binding phosphate, it blocks its absorption in the gut. Fewer pills. No mineral buildup. It’s not a cure, but it’s a step forward.Bottom Line
Antacids aren’t harmless. For someone with kidney disease, they’re a minefield. What seems like a quick fix for heartburn can lead to heart attacks, bone fractures, or even death. The good news? You don’t have to guess. Talk to your nephrologist. Know your numbers. Ask if your antacid is safe. There are better, safer options. You just need to ask for them.Can I take Tums if I have kidney disease?
You may take calcium carbonate (Tums) only under your nephrologist’s direction. In early-stage kidney disease (stage 3), it can be used as a phosphate binder at mealtime. In advanced stages (stage 4-5), it should be avoided as a daily binder. If you need it for heartburn, take it occasionally-no more than 1-2 tablets-and never within two hours of your phosphate binder. Always check your calcium levels monthly.
Is Milk of Magnesia safe for kidney patients?
No. Milk of Magnesia contains magnesium hydroxide. In kidney disease, your body can’t clear magnesium, and it builds up to toxic levels. Even small doses can cause muscle weakness, low blood pressure, and breathing problems. In dialysis patients, it’s led to cardiac arrest. Avoid it completely if your GFR is below 30 mL/min.
What’s the safest phosphate binder for kidney disease?
For most patients, sevelamer (Renagel) is the safest. It doesn’t contain calcium or aluminum, so it doesn’t raise blood calcium or risk aluminum toxicity. It’s more expensive than antacids, but studies show it lowers heart disease risk compared to calcium-based binders. Lanthanum carbonate and sucroferric oxyhydroxide are also good options, depending on cost and pill burden.
Can antacids cause kidney damage?
Antacids don’t directly damage the kidneys, but they can worsen kidney disease complications. High calcium from calcium antacids causes vascular calcification, which reduces blood flow to the kidneys. High magnesium can lead to heart failure and fluid overload. Aluminum toxicity can damage bone marrow and nerves. These complications make kidney disease harder to manage and accelerate decline.
How do I know if I’m taking too much calcium from antacids?
Symptoms include nausea, vomiting, constipation, increased thirst, frequent urination, confusion, and fatigue. But the only sure way is a blood test. Ask your doctor for a serum calcium level. If it’s above 10.2 mg/dL, you’re at risk for heart and blood vessel damage. Most patients don’t feel symptoms until levels are dangerously high.
Why don’t doctors always warn patients about antacid risks?
Many primary care doctors and pharmacists aren’t nephrology specialists. They see antacids as harmless OTC meds. Patients often don’t mention they have kidney disease unless asked. A 2022 study found 76% of CKD patients were never warned about antacid risks by their primary care provider. This is a communication gap-not a lack of evidence. Always bring up your kidney disease when getting any new medication.
Tatiana Bandurina
People still don’t get it. Tums isn’t candy. It’s a mineral bomb wrapped in a peppermint shell. I’ve seen three patients in the last year with calcium levels over 12 mg/dL because they thought 'it’s just for heartburn.' One had a heart attack at 54. No one warned them. No one asked if they had kidney disease. This isn’t about ignorance-it’s about systemic neglect. The FDA warning? Too little, too late.
And don’t even get me started on Milk of Magnesia. That stuff is liquid slow poison for anyone with GFR under 30. I’ve had to code someone because they took it for 'constipation'-like it’s a supplement. It’s not. It’s a cardiac timer.
Doctors don’t warn patients because they assume patients will read the label. But labels are written in lawyer-speak. And patients? They’re tired. They’re scared. They’re trying to survive. They don’t have the energy to decode pharmaceutical fine print.
Stop treating OTC meds like harmless. They’re not. They’re landmines with expiration dates.
And yes, I’m a nephrologist. And yes, I’m furious.
Philip House
Let’s be real-this whole thing is a scam. Big Pharma doesn’t want you using $10 antacids. They want you on $3,000/month binders so they can keep raking in cash. Sevelamer? It’s just a fancy name for calcium carbonate with a plastic coating. Same chemistry. Same effect. Just more expensive.
And who says aluminum is that dangerous? People in Japan used aluminum cookware for centuries. No dialysis dementia there. This fear-mongering is just corporate profit disguised as science.
Also, why are we treating kidney disease like it’s a death sentence? Maybe the real problem is that we’re overmedicalizing everything. A little high calcium? So what. Your body can handle it. Stop panicking over numbers on a screen.
And don’t even get me started on the 'nephrologist says' crowd. They’re the ones who told you to avoid salt for decades. Now we know that was nonsense. History repeats itself.
Jasmine Bryant
I had no idea antacids could mess with my thyroid meds. I take levothyroxine every morning and Tums whenever I get heartburn after lunch. My doctor never mentioned it. I just assumed it was fine since it’s OTC.
Just called my endo and she freaked out. Said my TSH has been creeping up for months and this could be why. She told me to stop taking Tums unless it’s at least 4 hours apart from my thyroid pill.
Also, I didn’t know calcium binders could calcify your arteries. I thought that was just from eating too much cheese. My GFR is 28. I’ve been taking Tums daily for 8 months. I’m terrified. I’m switching to sevelamer tomorrow. Wish me luck-this is gonna cost me a month’s rent.
Thanks for posting this. I think I just avoided a heart attack.
Sarvesh CK
The underlying issue here is not merely pharmacological but sociological. The commodification of healthcare has created a chasm between the patient’s lived experience and the clinical reality of their condition. The average individual, burdened by economic precarity and fragmented medical communication, is left to navigate a labyrinth of pharmaceutical options with minimal guidance.
Antacids, as affordable, accessible, and culturally normalized substances, become the default solution-not because they are optimal, but because alternatives are economically inaccessible. The moral imperative lies not in blaming patients for their choices, but in redesigning systems that render such choices necessary.
Prescription binders, while clinically superior, remain out of reach for millions. Until healthcare systems prioritize equity over profitability, we will continue to witness preventable tragedies disguised as individual negligence.
This is not a failure of knowledge. It is a failure of justice.
Moreover, the burden of education should not rest solely on the patient. Pharmacists, primary care providers, and public health campaigns must assume collective responsibility. The silence of the system is complicity.
Neil Ellis
Man, I used to pop Tums like M&Ms after spicy tacos. Never thought twice. Then my buddy got his GFR checked after a routine blood test-turned out he had stage 4 CKD. He’d been taking Tums daily for heartburn for 3 years. His calcium was through the roof. He needed a stent. His bones felt like chalk.
I didn’t know you could poison yourself with something you buy next to the gum at the gas station.
Now I tell everyone I know with diabetes, high blood pressure, or kidney issues: 'Don’t touch that bottle unless your doctor says yes.' It’s not just about kidneys-it’s about your whole damn body.
And yeah, I’m gonna start carrying a little card in my wallet that says 'I have CKD. Do not give me antacids.' Maybe it’ll save someone’s life.
Thanks for the heads-up. This is the kind of info that needs to go viral. Not cat videos. This.
Patrick Roth
Oh please. Aluminum toxicity? That’s 1990s fearmongering. I’ve been taking aluminum hydroxide for 12 years. I’m 68, on dialysis, and I’m fine. You think I’m gonna let Big Pharma scare me off a $12 bottle because some study says 'maybe'? I’ve got bills to pay and a family to feed.
And sevelamer? That’s a luxury item for rich folks with good insurance. Most of us can’t afford it. So we take what works. You think I want to be on a $2,000 pill? No. I want to live.
This article reads like a pharmaceutical ad. 'Use our expensive drug instead of the cheap one!' Newsflash: not everyone has a safety net.
Stop lecturing. Start solving.
Lauren Wall
Don’t take antacids if you have kidney disease. Period. End of story. Your life is more important than your heartburn.
And if you’re too lazy to read the label, you deserve what happens to you.
Brenda King
Thank you for this. I’m a stage 3 CKD patient and I had no idea calcium carbonate could be dangerous long-term. I’ve been taking 2 Tums after every meal because my doctor said 'it helps with phosphate.' I didn’t know they meant 'only if you’re monitored.'
I just got my bloodwork back-calcium was 10.5. I’m scared. I’m switching to sevelamer next week. It’s expensive, but I’d rather pay than end up in surgery.
Also-this is huge-my blood pressure meds stopped working last month. Turns out I was taking them 30 minutes after Tums. My doc said that’s why my numbers were all over the place.
So many people don’t know this. Please share this. Someone’s life could depend on it.
And yes, I cried reading this. Not because I’m weak. Because I’m grateful someone finally said it out loud.
arun mehta
Dear friends, this is not merely a medical issue-it is a profound human one. In the quiet corners of our homes, in the silent moments between meals and medications, countless individuals are making choices not out of ignorance, but out of necessity. The price of a pill should never determine the length of a life.
Let us not judge those who reach for Tums. Let us instead ask: Why is sevelamer unaffordable? Why are pharmacists not trained to ask about kidney function? Why do we treat mineral balance as a footnote rather than a cornerstone?
As someone who has walked beside loved ones through dialysis, I say this: Compassion must lead policy. Education must be free. Access must be universal.
And to those who suffer silently with high calcium or magnesium-your pain is valid. Your voice matters. Speak up. Ask for help. You are not alone.
🙏❤️