Heartburn hits hard - a burning sensation in your chest, sometimes rising to your throat, often after eating. If you’ve ever reached for a pill without a prescription, you’ve used an OTC heartburn medication. But not all of them work the same way, and using the wrong one can make things worse. There are three main types: antacids, H2 blockers, and proton pump inhibitors (PPIs). Each has a different speed, strength, and duration. Knowing which one fits your symptoms can save you from unnecessary discomfort - and potential side effects.
Antacids: Fast but Short-Lived Relief
Antacids are the oldest and simplest solution. They don’t stop acid production. Instead, they neutralize it - like pouring baking soda into vinegar. You feel relief fast: within 30 to 120 seconds. That’s why Tums, Rolaids, and Milk of Magnesia are go-tos for sudden heartburn after a spicy meal or a big slice of pizza.
Common ingredients include calcium carbonate (Tums), magnesium hydroxide (Milk of Magnesia), and aluminum hydroxide (Alternagel). A single Tums tablet contains 500-1,000 mg of calcium carbonate and can neutralize 12-24 mEq of acid. That’s powerful - but short-lived. The effect lasts only 30 to 60 minutes.
That’s the catch. If you’re getting heartburn every day or even a few times a week, antacids won’t cut it. You’ll be popping pills every hour. Plus, some people report rebound heartburn - the acid comes back stronger after 2-3 hours, especially with calcium-based antacids. That’s because the body overcompensates by producing even more acid.
They’re safe for occasional use, but don’t rely on them long-term. And don’t take them with other meds. Antacids can interfere with how your body absorbs antibiotics, thyroid pills, or iron supplements. Wait at least two hours after taking another medication before using an antacid.
H2 Blockers: Slower Start, Longer Lasting
H2 blockers work differently. Instead of neutralizing acid, they tell your stomach to make less of it. They block histamine, a chemical that signals your stomach cells to produce acid. Think of it like turning down the volume on a noisy speaker - not turning it off, but making it quieter.
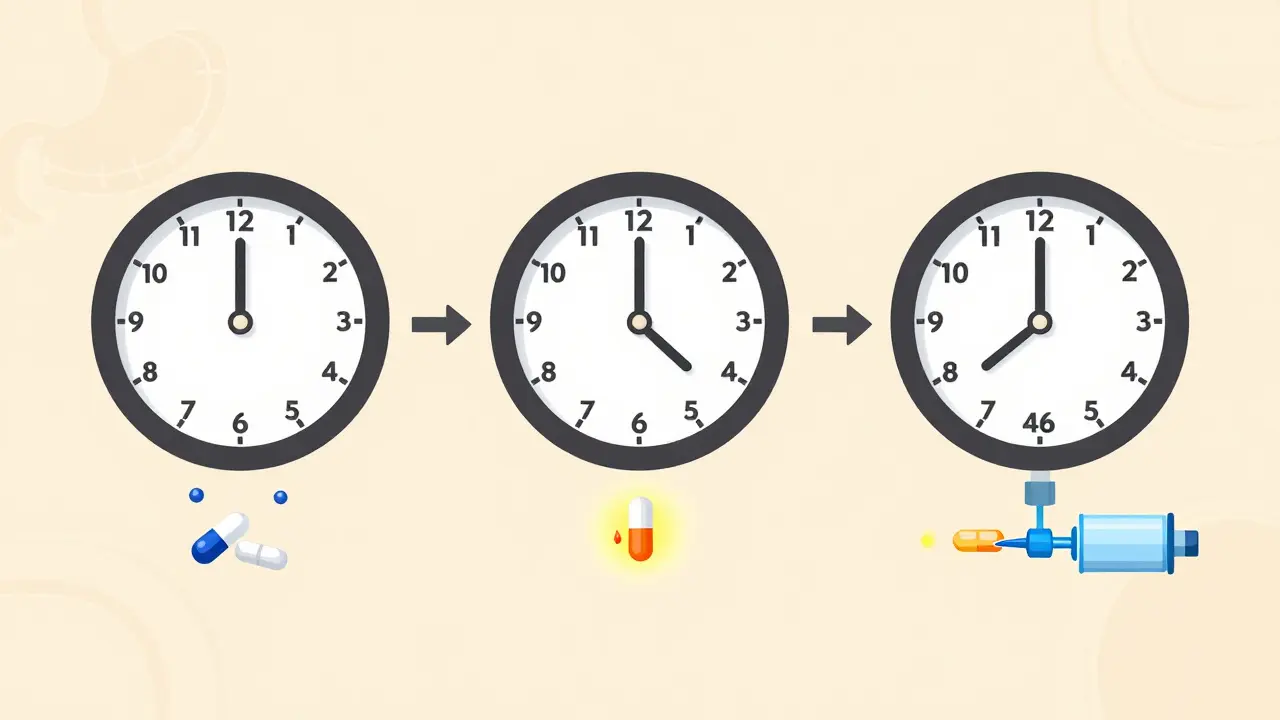
Popular OTC H2 blockers include famotidine (Pepcid AC), cimetidine (Tagamet HB), and nizatidine (Axid AR). They take longer to kick in - usually 60 to 180 minutes - so they’re not ideal for sudden heartburn. But once they work, they last 8 to 12 hours. That makes them perfect for planned situations: before a big dinner, after drinking coffee, or if you know you’ll lie down soon after eating.
Studies show H2 blockers reduce stomach acid by about 60-70%. That’s less than PPIs, but enough for people who get heartburn 1-2 times a week. They’re also better than PPIs for nighttime heartburn. One study found famotidine cuts nighttime acid by 75%, while omeprazole only hits 58%.
But there’s a downside. After 2-3 weeks of daily use, your body can start to adapt. The effect weakens. That’s called tachyphylaxis. If you’ve been taking Pepcid every night for a month and it’s not working like it used to, that’s why. It’s not broken - your body just got used to it.
Also, H2 blockers can interact with other drugs. Cimetidine, in particular, can interfere with blood thinners like warfarin or seizure meds like phenytoin. Always check with a pharmacist if you’re on other medications.
PPIs: The Heavy Hitters - But Not for Everyone
Proton pump inhibitors are the strongest OTC heartburn meds available. They shut down the acid-producing pumps in your stomach cells - the very last step in acid production. That’s why they reduce acid by 90-98%. That’s not just relief. That’s a full reset.
Common OTC PPIs include omeprazole (Prilosec OTC), esomeprazole (Nexium 24HR), and lansoprazole (Prevacid 24HR). All come in delayed-release tablets - meaning they’re coated to survive stomach acid and dissolve in the small intestine. That’s why you can’t crush them or take them with orange juice. The acid in the juice breaks down the coating, and the drug won’t work.
But here’s the thing: PPIs don’t work right away. It takes 24 to 72 hours to reach full effect. If you take one for sudden heartburn, you’ll be disappointed. They’re designed for daily, consistent use - taken 30 to 60 minutes before breakfast. That’s when the acid pumps are waking up. Taking them after a meal? You’re missing the window.
They’re the go-to for people with frequent heartburn - two or more days a week. A 2022 JAMA study showed PPIs reduced symptoms by 90% over 14 days, compared to 65% for H2 blockers. That’s a big difference.
But they come with real risks if used too long. The FDA has issued multiple warnings:
- Long-term use (over a year) is linked to a 35% higher risk of hip fractures.
- There’s a 1.7x higher chance of getting a serious gut infection called C. diff.
- Chronic use can lower magnesium levels - which can cause muscle cramps, irregular heartbeat, or seizures.
- Some users develop vitamin B12 deficiency after two or more years of daily use.
- There’s also a 1.8x higher risk of community-acquired pneumonia.
The FDA says: Don’t take PPIs for more than 14 days in a row without talking to a doctor. And don’t take them more than once every four months unless directed. Yet, 43% of users go past that limit. That’s not just common - it’s dangerous.
Which One Should You Use?
It’s not about what’s strongest. It’s about what matches your symptoms.
If you get heartburn once a week or less - maybe after a late-night taco - start with an antacid. Chew a Tums. You’ll feel better fast. No need to overcomplicate it.
If you know you’ll get heartburn after dinner, or you get it at night, try an H2 blocker. Take Pepcid AC 60-90 minutes before eating. It’ll keep your acid down through the night.
If you’re having heartburn two or more days a week - especially if it’s waking you up or interfering with meals - it’s time for a PPI. But only for 14 days. Then stop. If it comes back, see a doctor. Don’t just reach for another bottle.
Many people combine them. A 2023 survey found 68% of frequent heartburn sufferers use an antacid for instant relief and a PPI for long-term control. That’s smart - but only if you’re not masking a bigger problem.
What You Shouldn’t Do
Don’t use OTC heartburn meds as a crutch for poor habits. If you’re eating greasy food every night, drinking wine before bed, or lying down right after eating, no pill will fix that. Medications treat symptoms - not causes.
Don’t ignore warning signs. If you have trouble swallowing, vomiting blood, unexplained weight loss, or chest pain that spreads to your arm or jaw - that’s not heartburn. That could be a heart attack. Get checked.
Don’t assume generic is weak. Generic PPIs like omeprazole are bioequivalent to brand names like Prilosec. Curist and other generics now sell for under $5 a month - same effect, 80% cheaper.
Don’t take them with grapefruit juice or antacids at the same time. Both can ruin the PPI’s coating. Wait two hours between antacids and PPIs.
When to See a Doctor
OTC meds are great for occasional use. But if you need them more than twice a week for more than two weeks, it’s time to talk to a doctor. You might have GERD - gastroesophageal reflux disease - which needs a different approach.
Also, if you’re over 50 and have new heartburn symptoms, or if you’re taking NSAIDs like ibuprofen regularly, your risk of ulcers or stomach damage is higher. A doctor can check for H. pylori infection, Barrett’s esophagus, or other hidden issues.
The American Gastroenterological Association says: “PPIs are not meant to be a lifelong solution.” They’re a bridge - not a home.
Bottom Line
Antacids = fast, short fix. H2 blockers = steady, nighttime helper. PPIs = powerful, but only for short bursts. Pick the right tool for your symptom pattern. Use them as directed. Don’t overuse. And if you’re still struggling after 14 days, don’t keep reaching for the bottle - get help. Your stomach will thank you.
Oluwapelumi Yakubu
Antacids are like throwing water on a grease fire-works for a second, then the whole kitchen goes up in flames. I used to pop Tums like candy until I learned calcium carbonate tricks your stomach into making more acid. Now I just chew ginger and call it a night. No magic pills, just ancient wisdom.
Abhishek Mondal
Actually, your entire taxonomy is flawed-antacids don’t 'neutralize' acid; they buffer it, and the distinction matters in pharmacokinetics. Furthermore, the claim that PPIs reduce acid by '90–98%' is misleading without clarifying intragastric pH thresholds. The FDA’s warnings are statistically significant but contextually negligible for low-dose, short-term use. Also, why is grapefruit juice singled out? It’s not even a relevant interaction for PPIs-this article reads like a marketing brochure disguised as science.
melissa cucic
I appreciate the clarity of this breakdown, particularly the distinction between symptom relief and underlying pathology. It’s crucial to emphasize that PPIs are not a lifestyle accommodation-they are a medical intervention, and their overuse reflects a broader cultural tendency to pharmacologically manage discomfort rather than address root causes. I’ve seen patients on PPIs for over a decade, unaware of the nutrient deficiencies they’ve accumulated. Thank you for highlighting the 14-day limit.
Aaron Mercado
YOU PEOPLE ARE KILLING YOURSELVES WITH THESE PILLS!!! I knew a guy who took omeprazole for 5 years and ended up with osteoporosis and a C. diff infection that landed him in the ICU for 3 weeks-HE WAS 38!!! And now he’s on supplements, probiotics, and a vegan diet, and he’s fine-but he could’ve avoided it all if he’d just STOPPED EATING CHEESEBURGERS!!!
saurabh singh
Bro, this is gold! In India, everyone just chews neem leaves or sips ajwain water-but you’re right, if you’re having heartburn 5 days a week, you need to see a doc. I used to take Pantoprazole daily till my cousin told me, 'Bro, your stomach is not a machine you can reset with a button.' Now I eat early, avoid spicy stuff after 7 PM, and take 10 mins to walk after dinner. No pills. Just discipline. And yeah, generics? 10 bucks for a month’s supply here too. Same drug, zero drama.
John Wilmerding
Thank you for this exceptionally well-structured and evidence-based overview. I would like to add that the delayed onset of PPIs is not merely a pharmacokinetic quirk-it is a direct consequence of their mechanism of action: irreversible inhibition of the H+/K+ ATPase pump. New proton pumps must be synthesized for acid secretion to resume, which takes approximately 24–72 hours. This is why adherence to pre-meal dosing is non-negotiable. Additionally, the risk of hypomagnesemia is underrecognized; clinicians should consider serum magnesium levels in patients on long-term PPI therapy, especially those with concomitant diuretic use.
Chris Cantey
The real tragedy isn’t the PPIs. It’s that we’ve turned our bodies into machines to be fixed with buttons, when most of us just need to stop eating at midnight and get some sleep. I used to think heartburn was normal. Turns out, it was just me being lazy. No pill fixes bad habits. Just awareness. And silence.
Peyton Feuer
Also, don’t forget that antacids with aluminum can cause constipation, and magnesium ones? Diarrhea. So if you’re swapping between Tums and Milk of Magnesia, you’re basically playing stomach roulette. I just stick with one type now. And yeah, generic omeprazole? Total lifesaver. $3 at Walmart. No cap.