CCB Drug Interaction Checker
Check Your CCB Interaction Risk
Enter medications you're currently taking to see potential interactions with calcium channel blockers. This tool helps identify risks that may lead to dizziness, low blood pressure, or other serious side effects.
Interaction Assessment
Calcium channel blockers (CCBs) are one of the most commonly prescribed classes of heart and blood pressure medications. But behind their effectiveness lies a quiet danger: how they’re broken down in your body can change everything. A small change in another drug you’re taking, or even a glass of grapefruit juice, can push CCB levels into toxic territory. This isn’t theoretical-it’s happening every day in clinics and homes, especially among older adults on multiple medications.
What Calcium Channel Blockers Actually Do
CCBs work by blocking calcium from entering heart and blood vessel cells. Less calcium means relaxed blood vessels and slower heart rate. That’s why they’re used for high blood pressure, chest pain, and irregular heartbeats. But not all CCBs are the same. There are two main types: dihydropyridines (DHPs) like amlodipine, nifedipine, and felodipine; and non-dihydropyridines (non-DHPs) like verapamil and diltiazem.
DHPs mostly affect blood vessels. They lower blood pressure without slowing the heart much. That’s why amlodipine is the most prescribed CCB in the U.S.-it’s effective, long-lasting, and less likely to mess with heart rhythm. Non-DHPs like verapamil and diltiazem hit both the heart and blood vessels. They’re great for arrhythmias but come with more risks, especially when combined with other drugs.
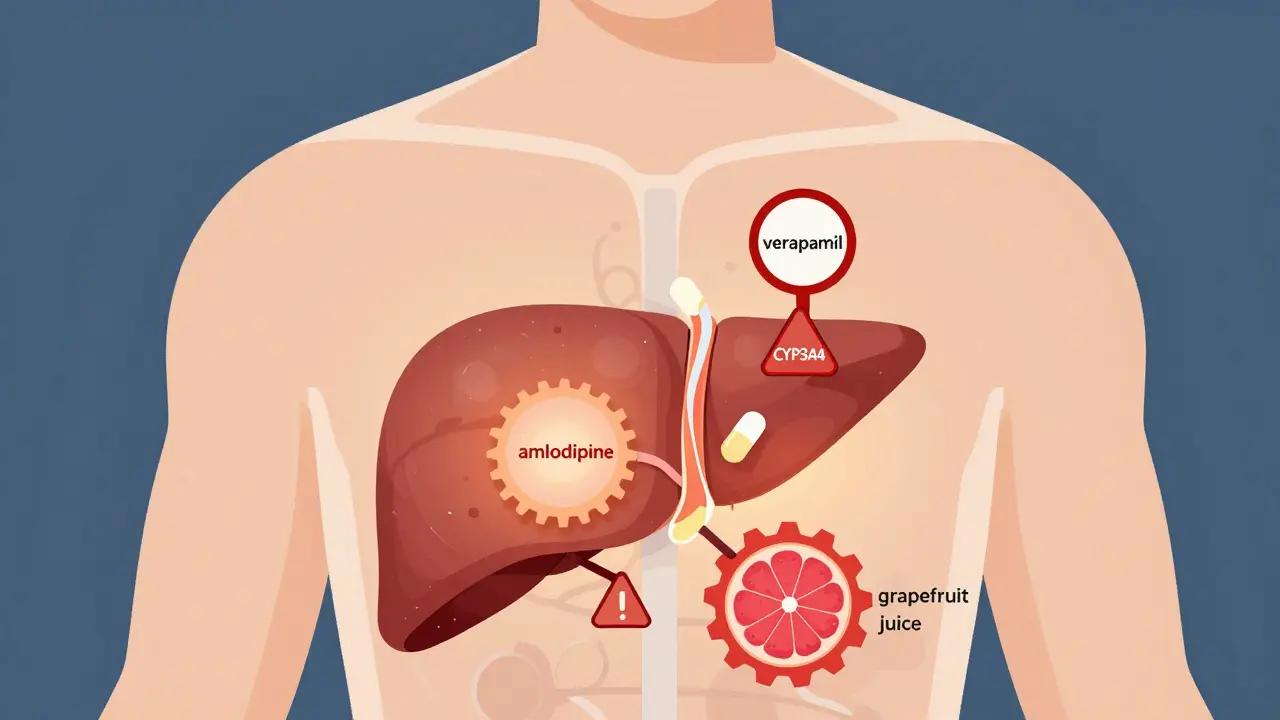
How Your Liver Breaks Down CCBs
Almost all CCBs are processed by the same enzyme in your liver: CYP3A4. This enzyme is like a factory worker that breaks down drugs so your body can flush them out. But here’s the catch: CYP3A4 is easily overloaded. If another drug or substance blocks or slows it down, CCBs build up in your blood. And because CCBs are highly protein-bound (90-99%), even a small increase in concentration can cause big effects.
Take amlodipine. It’s absorbed well, but only about 64% of the dose actually makes it into your bloodstream because of first-pass metabolism. Verapamil? Only 15-20% survives the liver. That’s why dosing is so sensitive. A 5 mg dose of amlodipine might be fine alone, but with a strong CYP3A4 inhibitor like ketoconazole, its levels can spike by 40%. For verapamil? That same combo can push levels up by 60-70%.
The Real Danger: Drug Interactions
It’s not just prescription drugs. Common substances like grapefruit juice, certain antibiotics, and antifungals can turn a safe CCB dose into a medical emergency.
- Grapefruit juice blocks CYP3A4 in the gut. A single glass can raise amlodipine levels by 30%, and verapamil by over 50%. In one study, 68% of patients who drank grapefruit juice while on CCBs developed dangerously low blood pressure.
- Antibiotics like clarithromycin and antifungals like itraconazole are strong CYP3A4 inhibitors. The FDA has issued multiple safety alerts about combining these with CCBs. Cases of severe bradycardia, heart block, and even cardiac arrest have been reported.
- Diltiazem doesn’t just get broken down by CYP3A4-it also blocks it. That means if you take diltiazem with simvastatin (a cholesterol drug), the statin levels can jump 400%. That’s a recipe for muscle damage and kidney failure.
- Verapamil also blocks P-glycoprotein, a transporter that moves drugs like digoxin out of cells. When combined, digoxin levels rise by 50-75%. That’s enough to cause fatal heart rhythms.
These aren’t rare cases. A review of 1,200 patient reports showed that 73% of negative experiences with CCBs were linked to drug interactions. The most common complaint? Unexpected dizziness or fainting-often from combining CCBs with erectile dysfunction meds like sildenafil. With verapamil, 87% of these cases caused dangerous drops in blood pressure. With amlodipine? Only 23%.

Why Age and Kidney Health Matter
As you get older, your liver and kidneys slow down. That means drugs stick around longer. Patients over 65 are 3.2 times more likely to have severe CCB interactions than younger adults. And if your kidneys aren’t working well (eGFR below 60 mL/min), the risk jumps another 47%.
Here’s the key difference: amlodipine is mostly cleared through the liver, so kidney problems don’t change its dosing. But verapamil? Even mild kidney impairment means you need a 50% dose reduction. Many doctors still miss this. Only 32% of community pharmacies check kidney function before prescribing verapamil.
Which CCB Is Safest for Complex Medication Regimens?
If you’re on five or more medications-common in older adults with heart disease, diabetes, and arthritis-your choice of CCB matters more than you think.
| CCB | CYP3A4 Substrate | CYP3A4 Inhibitor? | Half-Life | Interaction Risk | Recommended for Polypharmacy? |
|---|---|---|---|---|---|
| Amlodipine | Yes | No | 30-50 hours | Low | Yes |
| Verapamil | Yes | Yes | 4-12 hours | Very High | No |
| Diltiazem | Yes | Yes | 3-5 hours | High | Caution |
| Nifedipine | Yes | No | 2-5 hours (IR) | Moderate | Yes, if extended-release |
Based on real-world data, amlodipine is the safest bet for patients on multiple drugs. Only 12% of patients on amlodipine need a dose change when taking moderate CYP3A4 inhibitors. For diltiazem? That number jumps to 45%. And verapamil? The European Society of Cardiology says it should be avoided entirely if you’re on any CYP3A4 inhibitor. There are 17 documented cases of complete heart block requiring pacemakers from this combo.
What Doctors and Pharmacists Are Doing Now
Hospitals and clinics are waking up to this problem. The Cleveland Clinic now requires all new CCB prescriptions to be screened for CYP3A4 interactions. About 23% of patients are flagged as high risk. For those patients, guidelines recommend starting with amlodipine at 2.5 mg instead of 5 mg.
Pharmacists are spending an average of 12.7 minutes per CCB prescription checking for interactions. One in five prescriptions gets flagged and adjusted before being filled. Electronic health records now have automated alerts-Epic Systems reported a 42% drop in serious interactions after adding CCB-specific warnings in 2022.
In March 2023, the FDA approved the first tool called CCB-Check that integrates directly into hospital systems. It gives real-time risk scores based on your full medication list, age, kidney function, and liver health. In early trials, it cut hospitalizations from CCB interactions by 31%.
What You Should Do
If you’re taking a calcium channel blocker:
- Know which one you’re on. Amlodipine is the safest. Verapamil is the riskiest.
- Check every new medication. Even over-the-counter drugs, herbal supplements, or cold medicines can interact.
- Avoid grapefruit juice completely. No exceptions. It doesn’t matter if it’s fresh, frozen, or in a smoothie.
- Ask your pharmacist to run a drug interaction check. Most do it for free.
- Watch for signs of too much CCB: dizziness, fainting, swelling in ankles, slow heartbeat, extreme fatigue.
- If you’re over 65 or have kidney disease, ask your doctor if your dose needs adjusting. Many don’t check.
CCBs are powerful tools. But their power comes with responsibility. The goal isn’t just to lower blood pressure-it’s to do it without risking your life because of a hidden interaction. With the right knowledge and a little caution, you can stay safe and healthy.
Can I take grapefruit juice with a calcium channel blocker?
No. Grapefruit juice blocks the CYP3A4 enzyme in your gut, which is how your body breaks down most calcium channel blockers. This causes the drug to build up in your blood, leading to dangerously low blood pressure, dizziness, or fainting. This risk applies to all CCBs-amlodipine, verapamil, diltiazem, and nifedipine. Even a single glass can cause a reaction. It’s safest to avoid grapefruit juice entirely while taking any CCB.
Which calcium channel blocker has the fewest drug interactions?
Amlodipine has the fewest drug interactions among calcium channel blockers. It’s broken down by CYP3A4 but doesn’t inhibit the enzyme itself. That means it’s less likely to interfere with other medications. It also doesn’t affect P-glycoprotein, so it won’t raise levels of drugs like digoxin. For patients on multiple medications, especially older adults, amlodipine is the preferred choice because of its safety profile. Studies show only 12% of patients need a dose adjustment when taking moderate CYP3A4 inhibitors with amlodipine, compared to over 40% with diltiazem or verapamil.
Why is verapamil more dangerous than amlodipine with other drugs?
Verapamil is both a substrate and an inhibitor of CYP3A4, meaning it gets broken down by the enzyme but also blocks it. This dual role causes a double risk: other drugs can raise verapamil levels, and verapamil can raise levels of other drugs. It also blocks P-glycoprotein, which increases levels of digoxin, statins, and some anti-seizure meds. Studies show verapamil can increase digoxin levels by 50-75%, and simvastatin levels by over 400%. These interactions can cause heart block, muscle damage, or kidney failure. The European Society of Cardiology advises avoiding verapamil entirely if you’re taking any strong CYP3A4 inhibitor.
Do I need blood tests if I’m on a calcium channel blocker?
Routine blood tests aren’t needed for most people on CCBs. But if you’re taking verapamil with a CYP3A4 inhibitor, therapeutic drug monitoring may be recommended to keep verapamil levels between 50-150 ng/mL and avoid toxicity. If you have kidney disease, liver disease, or are over 65 and on multiple drugs, your doctor may check kidney function (eGFR) and liver enzymes (ALT, AST) every 3-6 months. Also, if you start a new medication or experience new symptoms like dizziness or swelling, ask your doctor if a blood test is needed.
Can kidney problems affect how calcium channel blockers work?
Yes, but it depends on the drug. Amlodipine is mostly cleared by the liver, so kidney problems don’t require a dose change. But verapamil is partly cleared by the kidneys. If your eGFR is below 60 mL/min, your doctor should reduce your verapamil dose by 50%. If your eGFR is below 30, verapamil may not be safe at all. Diltiazem also needs caution in kidney disease. Always tell your doctor if you have kidney issues before starting or changing any CCB.
Are there new tools to help avoid CCB interactions?
Yes. In 2023, the FDA approved CCB-Check, a tool that integrates with electronic health records to scan your full medication list and flag interaction risks in real time. It considers your age, kidney function, and liver health-not just drug names. Hospitals using it saw a 31% drop in hospitalizations from CCB interactions. Many pharmacies now use similar tools, and most EHR systems like Epic and Cerner have built-in alerts for CYP3A4 interactions with CCBs. If your doctor or pharmacist doesn’t mention these tools, ask if they’re being used.
What’s Next for Calcium Channel Blockers
The future of CCBs isn’t about new drugs-it’s about smarter use. Researchers are studying how your genes affect CYP3A4 activity. About 27% of people have genetic variants that make them slow or fast metabolizers. That means the same dose can be too little for one person and too much for another.
Even your gut bacteria matter. A 2023 study found gut microbiome differences explain 34% of the variation in how fast CCBs are cleared. That’s why two people on the same dose can have totally different responses.
By 2027, personalized dosing based on genetics, kidney function, and medication list will likely become standard. Until then, the safest approach is simple: know your drug, avoid grapefruit, tell your doctor everything you take, and choose amlodipine if you’re on multiple medications.
Tim Goodfellow
Whoa. I read this like a thriller novel. Grapefruit juice turning a simple blood pressure pill into a cardiac landmine? That’s wild. I used to chug it with my morning oatmeal like it was liquid gold. Guess I’m switching to orange juice now - and maybe thanking my liver out loud.
Elaine Douglass
This is so important for my mom shes 72 and on like 8 meds and just started amlodipine last month i told her to ditch the grapefruit smoothies but she said it tastes better than water
Alex Curran
Real talk amlodipine is the MVP here. I work in a geriatric clinic and we’ve switched 80% of our polypharmacy patients to it in the last year. Fewer ER visits fewer falls fewer confused grandpas wandering the halls wondering why they feel like they’re floating. It’s not sexy but it’s safe.
pascal pantel
Let’s be real this is just pharmacology 101 dressed up as a revelation. CYP3A4 inhibition is textbook. The fact that patients and even some clinicians are surprised by grapefruit interactions speaks volumes about the state of medical education. Also why is everyone acting like verapamil is some villain when it’s just a substrate and inhibitor? That’s not a flaw that’s its mechanism. Stop sensationalizing.
Nicole Rutherford
Of course the article picks amlodipine as the ‘safest’ because Big Pharma pushed it. They make billions off it. Meanwhile verapamil’s been around since the 70s and works better for arrhythmias. You’re just scared of side effects because you’ve never actually read the original studies. I’ve seen patients on verapamil for 20 years with zero issues. This is fearmongering.
Kelly Mulder
One must acknowledge the epistemological weight of this exposition. The CYP3A4 enzymatic pathway, while often oversimplified in lay discourse, remains the linchpin of pharmacokinetic integrity in calcium channel blockade. To conflate pharmacodynamic efficacy with metabolic vulnerability is not merely inaccurate-it is a categorical error. One must also interrogate the ontological implications of grapefruit juice as a pharmacological agent, wherein the furanocoumarins induce irreversible enzyme inhibition-a phenomenon that transcends mere ‘interaction’ and enters the realm of biochemical sabotage. The data presented, while statistically robust, lacks a critical hermeneutic lens on patient autonomy and the commodification of medical risk.
Dikshita Mehta
Great breakdown. I’m a pharmacist in India and we see this all the time. Elderly patients on multiple meds, no one checks interactions. We started using a free app called MedSafety Check and it flagged 3 out of 10 CCB prescriptions last month. Amlodipine is our go-to now. Also grapefruit juice? Absolutely banned in our counseling sheets. No exceptions.
Nina Stacey
I love how this post just lays it all out without drama. My dad was on diltiazem and started taking omeprazole and he kept passing out and no one knew why until his pharmacist said oh that’s a big no no and switched him to amlodipine and now he’s fine. I just wish more people knew this stuff. Like why is this not on every med bottle?
William Storrs
Hey if you’re on a CCB and you’re reading this you’re already ahead of the game. Knowledge is power here. Don’t be afraid to ask your pharmacist to run a full med check. They’re trained for this. And if you’re over 65? Tell your doctor you want to know if your kidney numbers are in the safe zone. Small steps save lives.
Takeysha Turnquest
We think we control our bodies but the liver? The gut? The enzymes? They’re the real architects. We pop pills like they’re candy and forget we’re dancing on a tightrope made of metabolic pathways. Amlodipine isn’t safer because it’s better-it’s safer because it doesn’t fight back. It just… exists. And maybe that’s the lesson. Sometimes the quietest thing is the most powerful.
Mark Able
Hey I just started amlodipine and I drink grapefruit juice every day. Is this gonna kill me? I don’t feel any different. Maybe you guys are overreacting?
Chris porto
It’s funny how we treat drugs like magic bullets. But the body’s not a machine. It’s a messy conversation between enzymes and food and genes and time. Amlodipine isn’t perfect. But it’s the least likely to start a fight. Maybe the real answer isn’t just which drug-but who’s taking it. And why. And what else they’re holding onto.
Kevin Motta Top
As someone who grew up in a family of pharmacists, I’ve seen this play out. My grandma took verapamil for years. Never had an issue. But she never took antibiotics or antifungals. Context matters. This isn’t about fear. It’s about awareness. Know your meds. Know your body. Simple.
William Liu
Just got prescribed amlodipine. Read this whole thing. Stopped my grapefruit smoothie. Told my mom. Told my uncle. This info needs to be everywhere. Thank you.