When your doctor prescribes a brand-name medication, you might expect to get exactly that - but what you actually walk away with at the pharmacy could be a completely different pill. That’s because of generic substitution, a routine but often misunderstood practice where pharmacies swap your brand-name drug for a cheaper generic version. It’s not a mistake. It’s not fraud. It’s policy. And if you don’t understand how it works, you could end up paying more, feeling worse, or getting caught in a bureaucratic loop that takes weeks to fix.
Generics aren’t knockoffs. They’re legally required to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. The FDA says they’re bioequivalent - meaning they work the same way in your body. But here’s the catch: bioequivalence doesn’t always mean identical experience. For some people, switching from brand to generic causes side effects, unstable blood levels, or even treatment failure - especially with drugs like warfarin, levothyroxine, or epilepsy medications. And insurance companies? They push hard for substitution because it saves them money. In 2023, generics made up 90% of all prescriptions filled in the U.S., but only 18% of total drug spending. That’s a $373 billion annual savings for the system - and a lot of pressure on patients to accept the switch.
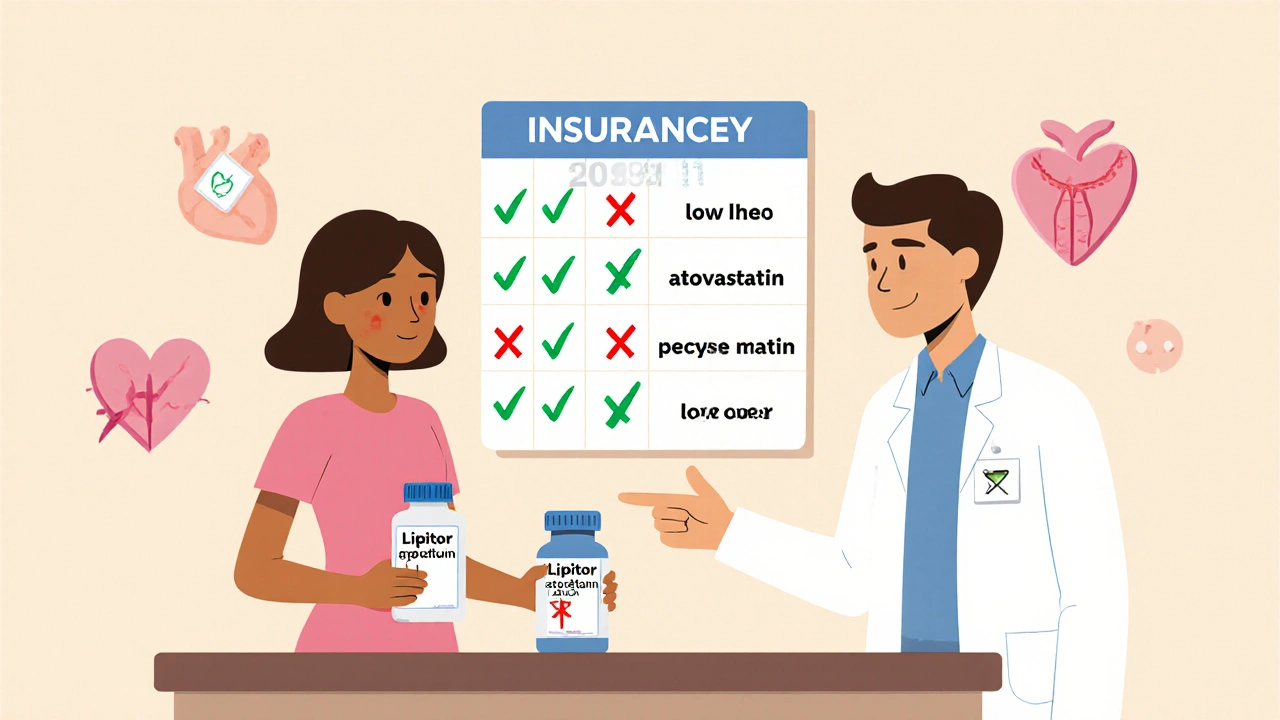
What Insurance Companies Require for Generic Substitution
Insurance plans don’t just encourage generic substitution - many mandate it. If your plan is like most private insurers in the U.S., you’ll pay less if you take the generic. If you insist on the brand, you’ll pay the difference out of pocket. Some plans go further: they won’t cover the brand at all unless your doctor proves it’s medically necessary. This is called a mandatory generic substitution policy.
For example, Sun Life Financial in Canada switched to mandatory substitution in 2012. Their data showed brand-name drugs cost $72 per claim on average - generics cost $27. That’s a 62.5% drop. In the U.S., pharmacy benefit managers (PBMs) like Express Scripts and CVS Caremark control 85% of these policies. They build formularies that list which drugs are covered and under what conditions. If your drug isn’t on the generic-preferred list, you’ll need prior authorization.
Here’s how it typically works:
- Your doctor writes a prescription for, say, Lipitor (atorvastatin).
- The pharmacy checks your insurance formulary and sees that atorvastatin (generic) is preferred.
- The pharmacist fills it with the generic unless the prescription says “Dispense as Written” or “Brand Medically Necessary.”
- If you get the generic, you pay your normal copay - maybe $5 or $10.
- If you want the brand, you pay the full price difference - sometimes $100+ extra per month.
Some insurers even make you pay the full retail price of the brand-name drug if you refuse the generic - no partial coverage. That’s why patients often don’t realize they’re being charged more until they get the bill.
State Laws That Control What Pharmacists Can Do
Insurance policies don’t act alone. They’re bound by state laws - and those vary wildly.
In 19 states, pharmacists are legally required to substitute generics unless the doctor says otherwise. In 7 states and Washington, D.C., the patient must give explicit consent before a substitution happens. In 31 states, the pharmacist must notify you - even if you don’t ask. And in 24 states, pharmacists have no legal protection if something goes wrong after a substitution.
Texas is one of the strictest. Their rules say a pharmacist can only substitute if:
- The generic costs you less than the brand (not just the insurer),
- You don’t refuse the switch,
- The doctor didn’t write “Dispense as Written” or “Brand Medically Necessary” on the prescription.
And they must use the FDA’s “Orange Book” to verify therapeutic equivalence. Only drugs rated “A” are eligible. That means no substitutions for drugs with complex delivery systems - like inhalers or injectables - unless they’re proven identical in every way, including the device.
For biologics - expensive, complex drugs like Humira or Enbrel - rules are even tighter. As of 2023, 38 states have laws governing biosimilar substitution. Thirty-two require the prescriber to be notified within 5-7 days. Twenty-seven require separate patient consent beyond what’s needed for regular generics. That’s because biosimilars aren’t exact copies - they’re “highly similar.” A small difference can matter more with these drugs.
When You Can Fight Back - And How
Just because your insurance wants you on a generic doesn’t mean you have to take it. You have rights.
The most powerful tool? The phrase “Dispense as Written” or “Brand Medically Necessary” written clearly on the prescription by your doctor. That’s it. That’s all it takes to block substitution in most states. But here’s the problem: many doctors don’t know this, or they don’t think it matters. They assume the pharmacist will follow the brand name.
Here’s what you need to do if you’ve had a bad experience with a generic:
- Go back to your doctor and explain what happened. Did your thyroid levels drop? Did you get headaches? Did your cholesterol spike? Write it down.
- Ask them to write “Dispense as Written” or “Brand Medically Necessary” on the prescription. Be specific. Don’t say “I don’t like it.” Say “I had unstable INR levels after switching from Synthroid to generic levothyroxine.”
- If your insurer denies coverage for the brand, file a prior authorization request. Most require documentation of prior treatment failure with the generic - lab results, symptom logs, or doctor notes.
- Keep copies of everything. Your pharmacy, your doctor, and your insurer all need the same paperwork.
Blue Cross Blue Shield of Michigan reports that 78% of prior authorization requests for brand-name drugs are approved when there’s solid medical evidence. Without it? You’re likely to get denied.
Why Some People React Differently to Generics
It’s not all in your head. Some people genuinely react worse to generics - not because the active ingredient is different, but because of the fillers, dyes, and binders.
Generic manufacturers use different inactive ingredients than brand-name makers. For most people, that’s harmless. But if you have allergies, sensitivities, or conditions like celiac disease, those additives can cause problems. One Reddit user reported severe bloating and fatigue after switching to a generic version of metformin - the active ingredient was the same, but the coating changed. Another user on Drugs.com said their migraines started after switching to a different generic of sumatriptan.
Even more confusing: two different generic versions of the same drug can behave differently. One might be made by Teva, another by Mylan. They’re both FDA-approved. But they’re not the same pill. If you’re stable on one generic, don’t switch to another without talking to your doctor. Insurers sometimes change which generic they cover to save money - and that can trigger side effects.
That’s why experts like Dr. Jerry Avorn from Harvard Medical School say: “For narrow therapeutic index drugs - where the difference between a safe dose and a toxic one is tiny - substitution should be done with caution.” That includes warfarin, lithium, phenytoin, and levothyroxine. The FDA says generics are safe for all these drugs. But real-world data tells a different story.
What to Do If You’re Forced to Switch
Let’s say you can’t fight the switch. Your insurance won’t cover the brand, and your doctor doesn’t think it’s necessary. You’re stuck with the generic. Here’s how to protect yourself:
- Ask your pharmacist which generic manufacturer they’re using. Write it down.
- Check your blood levels or symptoms within 2-4 weeks after switching. Don’t wait.
- If you feel off, don’t assume it’s “just adjustment.” Go back to your doctor with lab results.
- Keep a log: date, dose, symptoms, any changes in how you feel.
- If you’re on a chronic medication, ask your doctor to write a note for your file saying you’ve had issues with generic substitution in the past.
One patient on Reddit switched from brand-name Synthroid to generic levothyroxine and ended up with three dose adjustments over six months. Another switched from Lipitor to atorvastatin and saw no change - and saved $45 a month. Your experience could be either. But you won’t know unless you monitor it.

How to Avoid Surprises at the Pharmacy
Don’t wait until you’re standing at the counter to find out what you’re getting. Take control before you even fill the prescription.
- Call your insurance company and ask: “Is there a generic version of this drug? If so, is substitution mandatory?”
- Ask your doctor to write “Dispense as Written” on the script if you’ve had issues before.
- Check the pharmacy’s website - many list which generics they carry and their manufacturer.
- Use the FDA’s Orange Book app or website to look up your drug and see which generics are rated “A.”
- If you’re on Medicare Part D, remember: your plan’s formulary changes every January. Review it before the new year.
And if you’re ever unsure - ask the pharmacist. Not just “Is this generic?” but “Is this the same manufacturer as last time? Did my insurance approve this substitution?”
What’s Changing in 2025 and Beyond
The landscape is shifting. More complex drugs - like inhalers, injectables, and transdermal patches - are becoming available as generics. But substitution rates for these are still under 50% because they’re harder to replicate. The FDA is working on new guidelines for biosimilars, but experts predict state-level rules will stay messy through at least 2027.
Meanwhile, PBMs are pushing harder for substitution. More insurers are eliminating brand-name drugs from their formularies entirely. And as specialty drugs - which cost tens of thousands per year - grow in number, the pressure to use cheaper alternatives will only increase.
But here’s the bottom line: generic substitution isn’t going away. It’s here to stay. And it’s saving billions. But it’s not perfect. For some people, it works flawlessly. For others, it’s a health risk.
Your job isn’t to fight the system. It’s to navigate it. Know your rights. Know your drugs. Know your options. And never assume that “same active ingredient” means “same experience.”
Can a pharmacist substitute my brand-name drug without telling me?
In most states, pharmacists are required to notify you before substituting a generic drug - even if your doctor didn’t say “Dispense as Written.” Thirty-one states and Washington, D.C. have this requirement. But in 19 states, substitution is mandatory unless you or your doctor object. Always ask what you’re getting at the counter.
What does “Dispense as Written” mean on a prescription?
It means the prescriber is asking the pharmacist not to substitute a generic version. This phrase legally blocks substitution in nearly every state. If your doctor writes it, the pharmacy must fill the brand-name drug - even if it costs more. Some doctors use “Brand Medically Necessary” instead. Both mean the same thing.
Why does my insurance only cover the generic version?
Insurers use formularies to control costs. Generics cost 80-90% less than brand-name drugs. By requiring you to use the generic, they save money - and often pass some of that savings to you in lower copays. If you choose the brand, you pay the full price difference. This is called “mandatory generic substitution.”
Can I get the brand-name drug if I pay the difference?
Yes - but only if your doctor writes “Dispense as Written” or “Brand Medically Necessary.” Even then, your insurance won’t pay for the brand. You’ll pay the full retail price of the brand minus what the generic would have cost. That difference can be $50, $100, or more per month.
Are generic drugs less effective than brand-name drugs?
The FDA says generics are just as effective. But real-world experience shows mixed results. For most people, they work the same. For others - especially with narrow therapeutic index drugs like levothyroxine or warfarin - switching can cause instability. Differences in inactive ingredients, manufacturing processes, or even the pill’s coating can affect how the drug is absorbed. Monitor your symptoms and lab results after any switch.
Amie Wilde
Just got switched to a generic for my thyroid med and my heart started racing. Didn’t even know I could fight it until I read this. Doc didn’t say anything. Now I’m printing this out and taking it to my next appointment.
Gary Hattis
As someone who’s lived in 5 countries, this is wild. In India, generics are the default and no one bats an eye. In Germany, you have to sign a waiver to get the brand. Here? It’s a legal gray zone with pharmacy staff playing insurance enforcers. We need national standards, not 50 different state rulebooks.
Samantha Wade
It is imperative to recognize that the pharmacological equivalence of generic medications, as defined by the FDA, does not inherently guarantee clinical equivalence across all patient populations. The variability in inactive ingredients-such as lactose, dyes, and binding agents-can precipitate adverse reactions in individuals with sensitivities, particularly those with autoimmune or gastrointestinal disorders. Documentation of such reactions, coupled with laboratory data, is not merely advisable-it is clinically essential for securing prior authorization and preserving therapeutic stability.
Elizabeth Buján
My mom switched to generic Lipitor and started getting these crazy muscle cramps. She thought it was just getting older. Turns out? It was the filler. She went back to brand and within two weeks she was walking like a 40-year-old again. I’m so glad this post exists. So many people think it’s all in their head when it’s really the pill’s coating. Please, if you feel weird after a switch-don’t ignore it. Your body’s not lying.
Andrew Forthmuller
Wait so if my doc writes ‘dispense as written’ they can’t swap it? Even if my insurance hates it? That’s it? No other steps? That’s kinda wild.
vanessa k
I’ve been on levothyroxine for 12 years. Switched generics three times. Each time my TSH went haywire. I stopped trusting the system. Now I pay out of pocket for Synthroid. It’s $120 a month. Worth every penny. My anxiety dropped, my energy came back. No one should have to gamble with their health for a $5 copay.
manish kumar
As a pharmacist in rural India, I’ve seen how generic substitution saves lives here-where people can’t afford brand drugs at all. But I also see the confusion when patients come back with side effects after switching. The problem isn’t the generic-it’s the lack of patient education. In the U.S., you have access to labs, doctors, and formularies. Use them. Ask your pharmacist for the manufacturer name. Write it down. Track your symptoms. Knowledge is power. And if your doctor doesn’t know about ‘Dispense as Written,’ teach them. We’re all in this together. The system isn’t broken-it’s just not designed for the patient’s voice. Start speaking up.
Nicole M
My insurance changed my generic from Teva to Mylan last month. I didn’t notice until my migraines came back. Turned out the coating was different. Now I always ask the pharmacist: ‘Same as last time?’ If they say no, I say no. It’s not worth the headache. Literally.