Opioid-Antihistamine Safety Checker
Check if your opioid pain medication and antihistamine are safe to take together. This tool identifies dangerous combinations that can cause life-threatening breathing problems.
Result
When you're in pain and your nose is running, it’s easy to reach for a painkiller and an allergy pill at the same time. But combining opioids with antihistamines isn’t just a minor inconvenience-it can be life-threatening. This isn’t theoretical. People are ending up in the ICU, on ventilators, or worse because they didn’t know these two common medications could team up to shut down their breathing.
Why This Combination Is So Dangerous
Opioids like oxycodone, hydrocodone, and morphine work by binding to receptors in your brain that control pain. But they also slow down your breathing. That’s a known side effect, and doctors warn about it. But here’s what many don’t realize: first-generation antihistamines-like diphenhydramine (Benadryl), hydroxyzine (Atarax), and doxylamine (Unisom)-do the exact same thing. They cross into your brain, block histamine, and make you drowsy. That drowsiness isn’t just "feeling sleepy." It’s a direct suppression of your brain’s drive to breathe. These two drugs don’t just add up-they multiply. One study found that patients taking opioids alone had a 0.7 in 10,000 chance of dying from respiratory depression. When benzodiazepines were added, that risk jumped tenfold. While similar large-scale numbers for antihistamines aren’t as widely published, the mechanism is identical. The American Academy of Family Physicians reports sedation occurs in 20% to 60% of opioid users. Add a sedating antihistamine, and that number doesn’t just rise-it skyrockets.It’s Not Just Prescription Drugs
The biggest danger isn’t from prescriptions. It’s from the stuff you buy without one. Diphenhydramine is in sleep aids, cold medicines, and allergy pills. Hydroxyzine is prescribed for anxiety and itching, but many patients don’t connect it to their opioid pain meds. A 68-year-old man in North Carolina ended up in the ICU after taking hydrocodone for back pain and Benadryl for itching. He was unresponsive for 36 hours. His doctor didn’t warn him. Neither did the pharmacist. He didn’t even think to mention the Benadryl. Over-the-counter doesn’t mean safe. A 2021 survey by the National Institutes of Health found that 68% of patients don’t tell their doctors what OTC meds they’re taking. Why? Because they assume it’s harmless. But when you mix it with an opioid, it’s not harmless. It’s a silent killer.Who’s Most at Risk
This isn’t a risk for everyone equally. Certain groups are far more vulnerable:- Elderly patients: Their bodies process drugs slower. Their brains are more sensitive to sedation. The Beers Criteria, used by geriatric specialists, lists diphenhydramine and hydroxyzine as "potentially inappropriate" for older adults because of their anticholinergic effects.
- People with COPD or sleep apnea: If your lungs are already struggling, adding a drug that slows breathing is like turning off the air pump. Studies show OIRD (opioid-induced respiratory depression) happens most often in the first 24 hours after surgery-and mostly in those with pre-existing lung or heart conditions.
- Those on high opioid doses: The higher the opioid dose, the greater the risk. But even low doses become dangerous when paired with a strong sedative.

What Makes Antihistamines Worse Than Other Sedatives
You’ve probably heard about the dangers of mixing opioids with benzodiazepines. That’s true. But antihistamines are sneakier. There’s no antidote. If someone overdoses on a benzodiazepine, doctors can give them flumazenil. If they overdose on an antihistamine? There’s nothing. You can’t reverse the sedation. You can only support breathing until the drug wears off-which can take hours or even days. Also, second-generation antihistamines like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) have almost no brain penetration. That means they don’t cause the same sedation. But most people don’t know the difference. They see "antihistamine" on the label and assume they’re all the same. They’re not.Real Cases, Real Consequences
A woman on PatientsLikeMe fractured her hip after falling asleep while taking hydroxyzine and oxycodone. She didn’t realize the combo made her so drowsy she couldn’t get up. Another patient, documented by the Institute for Safe Medication Practices, died after combining codeine with diphenhydramine. In a six-month survey of 147 cases among doctors on Sermo, 32% of patients needed naloxone-the opioid reversal drug-just to stay alive. These aren’t rare. They’re predictable. And they’re preventable.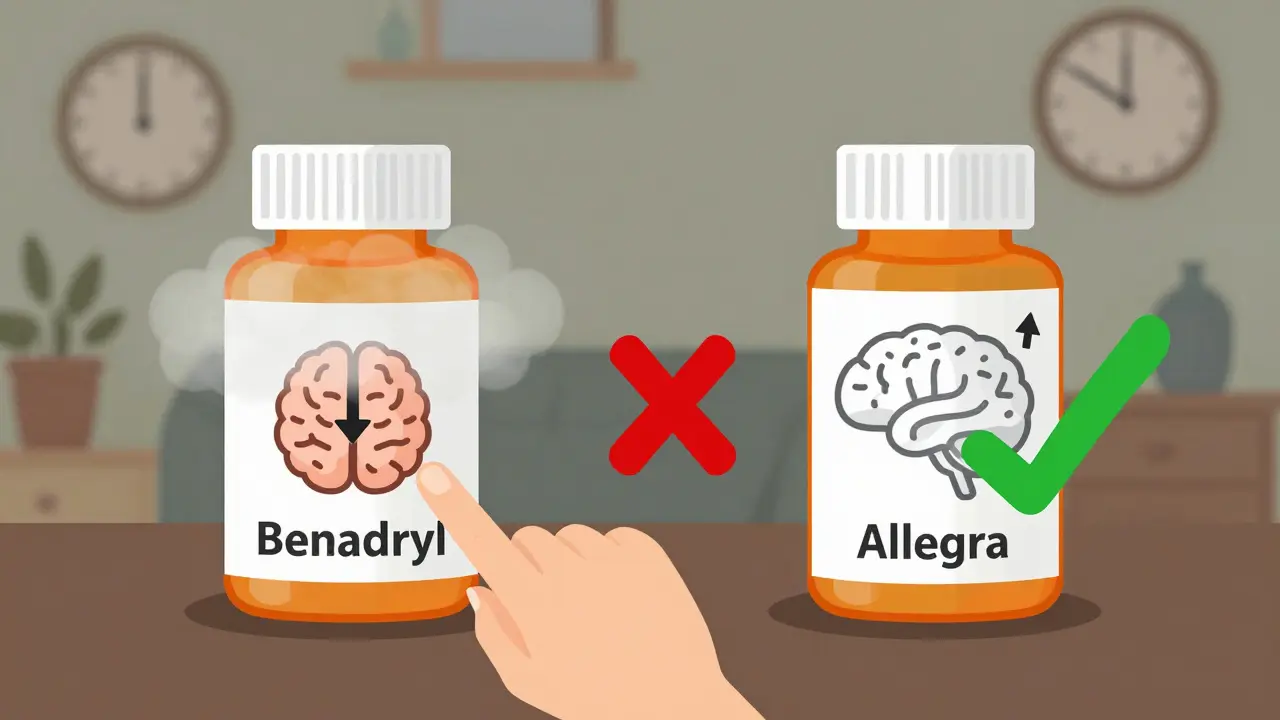
What Doctors and Pharmacies Are Doing About It
Hospitals and clinics are starting to catch on. Epic Systems, the biggest electronic health record provider in the U.S., now triggers "hard stop" alerts when a doctor tries to prescribe an opioid with a sedating antihistamine. Over 90% of U.S. hospitals using Epic have this feature. The University of Michigan cut adverse events by 42% after adding these alerts. The FDA updated its opioid safety guidelines in May 2023 to explicitly include all CNS depressants-not just benzodiazepines. The REMS program now requires 1.4 million prescribers to complete updated training on drug interactions by the end of 2023. Pharmacists are required to hand out medication guides with every opioid prescription that warn about combining with other sedatives. But here’s the problem: these alerts only work if the doctor knows what the patient is taking. And most patients don’t tell them.What You Can Do
If you’re on an opioid:- Don’t take any antihistamine without asking. Not even Benadryl. Not even for allergies or sleep.
- Switch to a non-sedating antihistamine. Fexofenadine (Allegra), loratadine (Claritin), or cetirizine (Zyrtec) are safe alternatives. They work just as well for allergies without the brain fog or breathing risk.
- Always list every medication you take. Include supplements, OTC pills, and even herbal teas. Many people forget melatonin or valerian root-those also depress the CNS.
- Ask your pharmacist. They’re trained to spot dangerous combos. If they don’t warn you, ask: "Could this interact with my pain medicine?"
- Watch for signs of too much sedation. Slurred speech, confusion, slow breathing (less than 10 breaths per minute), or being hard to wake up are red flags. Call 911 immediately.
The Bottom Line
You don’t need to avoid opioids or antihistamines entirely. But you need to understand how they work together. The risk isn’t in taking one or the other. It’s in taking both without knowing the consequences. This isn’t about fear. It’s about awareness. Every year, hundreds of people die because they thought a little extra sleep aid wouldn’t hurt. It does. And it can happen to anyone-even if you’re young, healthy, and think you’re fine. Talk to your doctor. Ask questions. Don’t assume. Your life depends on it.Can I take Benadryl with my opioid painkiller?
No. Benadryl (diphenhydramine) is a first-generation antihistamine that strongly crosses into the brain and slows breathing. When combined with opioids, it can cause extreme drowsiness, dangerously slow breathing, coma, or death. Even one dose can be risky, especially if you’re elderly or have lung problems.
Are all antihistamines dangerous with opioids?
No. Only first-generation antihistamines like diphenhydramine, hydroxyzine, and doxylamine are risky because they affect the brain. Second-generation antihistamines like fexofenadine (Allegra), loratadine (Claritin), and cetirizine (Zyrtec) have minimal brain penetration and are generally safe to use with opioids. Always check the active ingredient on the label.
What should I do if I’ve already taken both?
If you’ve taken both and feel unusually drowsy, confused, or have slow or shallow breathing, call 911 immediately. Don’t wait. Don’t try to sleep it off. Opioid and antihistamine overdose can lead to respiratory arrest within minutes. If you have naloxone on hand, use it-it won’t reverse the antihistamine, but it can help with the opioid component while you wait for emergency help.
Why don’t doctors warn me about this?
Many do-but not all. A CDC report found only 34% of patients prescribed opioids receive full counseling about drug interactions. Some doctors assume patients know, others don’t realize how common OTC antihistamine use is. If you’re on an opioid, ask directly: "Are there any medications I should avoid?" Don’t wait for them to bring it up.
Is this risk higher with fentanyl or other strong opioids?
Yes. Fentanyl is 50 to 100 times more potent than morphine. Even small doses can cause respiratory depression. When paired with a sedating antihistamine, the risk multiplies. Synthetic opioids like fentanyl are now involved in over 80% of opioid-related deaths in the U.S. Combining them with any CNS depressant dramatically increases the chance of fatal overdose.
Can I use a sleep aid if I’m on opioids?
Most over-the-counter sleep aids contain diphenhydramine or doxylamine-both are dangerous with opioids. Instead, talk to your doctor about non-sedating options like melatonin (in low doses), cognitive behavioral therapy for insomnia (CBT-I), or adjusting your opioid schedule. Never use sleep aids without approval.

Christina Bischof
Been there. Took Benadryl for allergies while on oxycodone after surgery. Woke up on the floor next to my coffee table. Didn’t even remember falling. Never again.
Melissa Taylor
This is so important. I work in ER and see this way too often. People think OTC means harmless. It’s not. A simple diphenhydramine can turn a manageable situation into a code blue. Doctors need to be louder about this.
RONALD Randolph
Why is this even a discussion? You’re an idiot if you mix CNS depressants. The FDA has warnings on the bottles. The pharmacist hands you a pamphlet. If you still do it, you deserve what you get. Stop being lazy and read the damn label.
Raj Kumar
in india we dont even know what antihistamine is called. people just buy whatever is cheap and takes away the itch. no one tells them. no one cares. this is a global problem.
John Brown
My grandma took hydroxyzine for anxiety and oxycodone for arthritis. She didn’t even realize they were interacting. She started nodding off at dinner. We switched her to Zyrtec and she’s been fine. Just ask your pharmacist. It’s free advice that could save your life.
John Samuel
Let’s not sugarcoat this: the pharmaceutical industry profits from ignorance. They sell you the opioid. They sell you the antihistamine. They profit from both. But when the system fails to warn you? That’s not negligence. That’s systemic malice disguised as convenience.
And yet, we’re still surprised when people die from ‘over-the-counter’ meds? Wake up. The system isn’t broken-it’s designed this way.
It’s not about individual responsibility. It’s about institutional accountability. If your EHR doesn’t auto-flag this interaction, it’s not a glitch. It’s a feature.
And if your doctor doesn’t bring it up? They’re not busy. They’re complacent.
People don’t die because they’re careless. They die because the system gave them every reason to believe it was safe.
Next time you see a patient on opioids, ask: ‘What else are you taking?’ Not ‘Do you take anything else?’ Ask it like your life depends on it. Because it does.
This isn’t a cautionary tale. It’s a indictment.
And until we treat this like the public health emergency it is, more people will die. Quietly. Alone. And completely preventable.
Cassie Henriques
As a pharmacist, I see this daily. Patients say ‘I only took one’ like it’s a tiny thing. But diphenhydramine + opioid = synergistic CNS depression. It’s not additive-it’s multiplicative. And no, Zyrtec isn’t always the answer-some patients develop tolerance to it. We need better education at the point of sale.
Also, melatonin isn’t risk-free either. It’s not a CNS depressant per se, but it can potentiate sedation in polypharmacy cases. Always disclose everything-even ‘natural’ stuff.
And yes, I’ve had patients yell at me for ‘scaring them’ with warnings. I don’t care. I’d rather lose a sale than a life.
Jake Sinatra
It’s staggering how many people still believe OTC equals safe. The CDC data is clear: opioid-related deaths involving antihistamines have increased 300% since 2015. This isn’t anecdotal. It’s epidemiological. We need mandatory patient education modules tied to opioid prescriptions. Not optional. Mandatory.
And if you’re a clinician and you’re not screening for OTC use, you’re not doing your job.
Benjamin Glover
Of course it’s dangerous. Everyone knows this. The only people who don’t are the ones who don’t read. This isn’t a public health crisis. It’s a failure of personal responsibility.
Mike Nordby
One of the most overlooked aspects is the elderly. They’re often on multiple meds, have slower metabolism, and are more sensitive to anticholinergics. The Beers Criteria exists for a reason. Yet, so many primary care docs still prescribe Benadryl to seniors for sleep. It’s outdated. Dangerous. And frankly, lazy.
Non-pharmacological sleep hygiene should be the first line-not a pill with 40 years of bad data behind it.
This isn’t just about opioids. It’s about how we treat aging.
Sai Nguyen
Americans think they can medicate everything. You have allergies? Take Benadryl. Can’t sleep? Take Benadryl. In pain? Take oxycodone. Then wonder why you’re dead. This is what happens when you treat your body like a vending machine.
Michelle M
It’s not just about the drugs. It’s about how we’ve normalized self-medication. We don’t trust our bodies anymore. We don’t sit with discomfort. We reach for the next pill. And when two pills combine to silence your breath? We call it an accident. But it’s not. It’s the end result of a culture that equates relief with consumption.
Maybe the real danger isn’t the combination-it’s the belief that we need to fix everything with chemistry.
What if the answer isn’t more warnings? But more presence? More listening? More patience with pain?
I don’t have the answers. But I know this: no pill should ever be the first response to being human.
Jocelyn Lachapelle
My brother died from this. He was 32. Healthy. Took hydrocodone after a car accident and Benadryl for a rash. No one told him. The ER said he had ‘unexplained respiratory arrest.’ We only found out later from his pharmacy records. I wish I could go back and shake him. Or shake the doctor. Or shake the pharmacist. But I can’t. So I’m telling you now: if you’re on opioids, don’t touch anything that makes you sleepy. Not even once. Not ever.