Medication-Food Interaction Checker
Check if your medication interacts with food and learn the proper timing for safe and effective treatment.
Medication Interaction Results
Ever taken a pill and wondered why it didn’t work-or why you felt worse after eating? It’s not just in your head. What you eat can change how your medicine works, sometimes in dangerous ways. This isn’t about fancy diets or strict rules. It’s about simple, practical choices that keep your meds working right and your body safe.
Why Food Matters More Than You Think
Your stomach isn’t just a bag for food. It’s a chemical factory. When you eat, your body changes its pH, releases enzymes, and shifts blood flow-all of which can mess with how your medicine gets into your system. About 30% of bad reactions to medications come from food interactions, not mistakes in dosage. That’s not rare. That’s common.
Some foods make drugs stronger. Others make them weaker. A few can even cause new side effects you didn’t know existed. The good news? You don’t need to become a nutritionist. You just need to know a few key rules.
Three Ways Food Changes Your Medicines
There are three main ways food and medicine interact:
- Absorption: Food can block your body from absorbing the drug. Think of it like a door that’s locked when you eat.
- Metabolism: Some foods change how your liver breaks down the drug, making it stick around too long-or disappear too fast.
- Effect: Food can directly cancel out or boost the drug’s action in your body, like vitamin K fighting warfarin.
It’s not just about what you eat. It’s about when you eat it.
Medicines That Hate Food
Some drugs work best on an empty stomach. That means 1 hour before or 2 hours after eating. If you take them with food, you might get half the benefit-or none at all.
- Levothyroxine (for thyroid): Take it first thing in the morning, before coffee, before breakfast. If you eat even 30 minutes after, your body absorbs 34% less. That’s enough to make your fatigue worse.
- Tetracycline antibiotics: Dairy products like milk, cheese, and yogurt bind to this drug like glue. If you take it with yogurt, you’re only getting half the dose. Wait 2 hours before or 4 hours after dairy.
- Penicillin G: Food lowers its absorption by 40-60%. Take it on an empty stomach, even if your stomach feels a little upset.
These aren’t suggestions. They’re science-backed timing rules. Skip them, and your treatment fails.
Food That Makes Drugs Too Strong
Some foods don’t just block drugs-they turn them into overdrive.
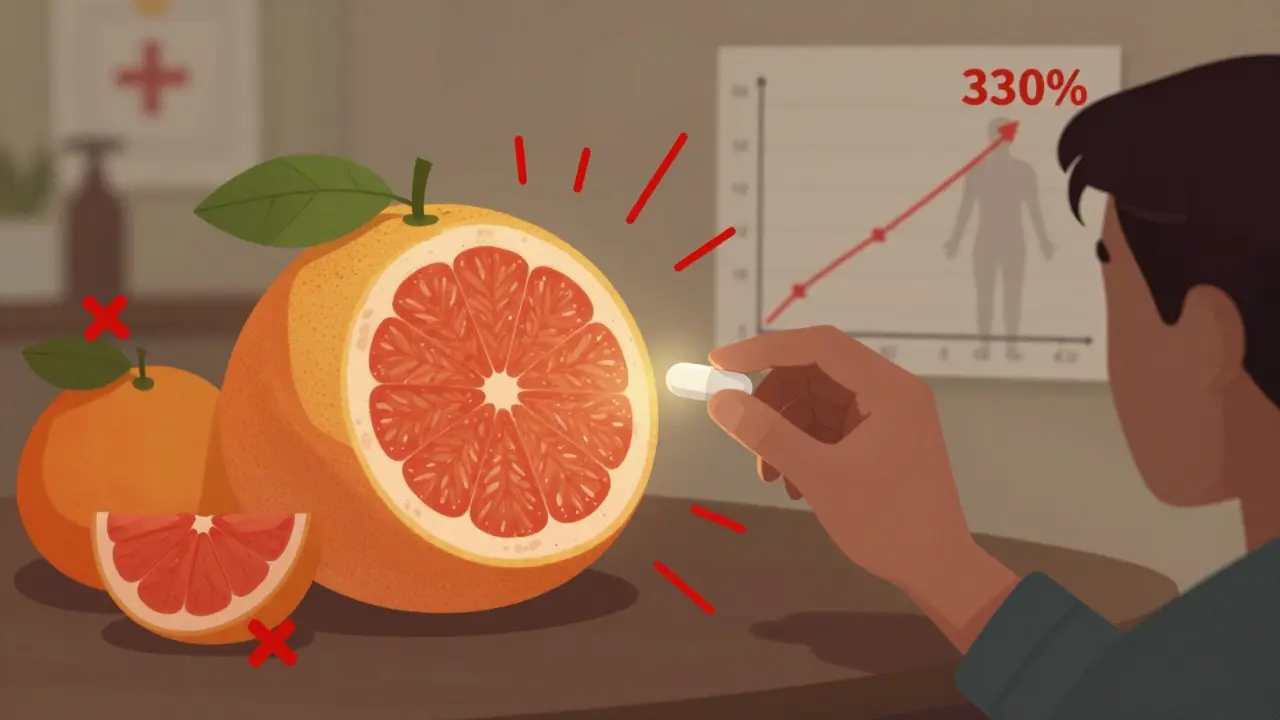
Grapefruit juice is the most dangerous example. It blocks an enzyme in your gut called CYP3A4, which normally breaks down certain drugs. When that enzyme is shut down, the drug builds up in your blood like a traffic jam.
- Simvastatin (a statin for cholesterol): Grapefruit juice can raise blood levels by 330%. That’s not just stronger-it’s risky. Muscle damage, kidney failure, even death can happen.
- Some blood pressure pills and anti-anxiety drugs also react badly. If your pill bottle says “avoid grapefruit,” don’t test it.
It’s not just grapefruit. Pomelo, Seville oranges, and some hybrid citrus fruits do the same thing. If you’re on a statin, skip all of them.
Food That Neutralizes Your Medicine
Some foods don’t make drugs stronger-they cancel them out.
Warfarin (a blood thinner) is the classic case. It works by blocking vitamin K, which helps your blood clot. But if you eat a big salad one day and no greens the next, your blood clotting changes unpredictably. That’s dangerous.
The fix? Consistency. You don’t have to avoid spinach or kale. Just eat about the same amount every day. If you normally eat one cup of cooked spinach, keep doing that. If you eat none, keep doing that. A variation of more than 10-15% can cause dangerous INR swings. People who use food diaries have 28% fewer problems.
Other foods that affect warfarin: cranberry juice, green tea, and large amounts of mango. Don’t assume they’re harmless.
Food That Helps Your Medicine
Not all food is the enemy. Sometimes, eating with your medicine makes it safer-or even better.
- NSAIDs like ibuprofen: Taking them on an empty stomach gives you a 15% chance of a stomach ulcer. Take them with food? That drops to 4%. Food protects your stomach lining.
- Diazepam and griseofulvin: These drugs are fat-soluble. Take them with a meal that has some fat-like eggs, avocado, or peanut butter-and your body absorbs 25-35% more.
- Omeprazole: This acid-reducing pill works best taken 30-60 minutes before your first meal. Food triggers acid production, and the drug needs to be in place before that happens.
Don’t assume all meds should be taken with food. Know which ones need it-and which ones don’t.
What About Alcohol and Caffeine?
Alcohol doesn’t just make you dizzy. It can:
- Boost drowsiness from painkillers or anxiety meds
- Damage your liver when taken with acetaminophen
- Raise blood pressure when mixed with some blood pressure drugs
Even one drink can be risky. If your doctor didn’t say it’s okay, assume it’s not.
Caffeine? It can interfere with some asthma meds and ADHD drugs, making them less effective. It can also raise heart rate when taken with decongestants. A cup of coffee isn’t a problem for most-but if you’re on multiple meds, check.
What You Should Do Right Now
You don’t need to memorize a list of 50 drugs. Here’s what to do instead:
- Ask your pharmacist every time you get a new prescription: “Does food affect this? When should I take it?”
- Read the label. If it says “take on empty stomach,” “avoid grapefruit,” or “take with food,” write it down.
- Use a simple schedule. Put your meds next to your toothbrush or coffee maker. Link them to daily habits: “After brushing my teeth, I take my thyroid pill.”
- Track your diet if you’re on warfarin. Use a free app or just a notebook. Write down how much spinach, kale, or broccoli you eat each day.
- Never mix meds with grapefruit. Not even a sip. Not even “once in a while.”
Patients who follow these steps reduce medication errors by nearly half. That’s not magic. That’s just paying attention.
Why This Matters More Than You Realize
Every year, food-drug interactions send over 1,100 people to the ER just because of grapefruit. Thousands more are hospitalized because they took their antibiotic with milk or skipped their warfarin timing.
It’s not about being perfect. It’s about being aware. You don’t need to stop eating your favorite foods. You just need to know when to eat them-relative to your pills.
The FDA now requires clearer labels on new drugs. Pharmacies are required to counsel seniors on food interactions. But until you know the basics, you’re still at risk.
Medicine works best when your body is predictable. Food is part of that. Don’t let it sabotage your health.
Can I take my medication with a glass of milk?
It depends on the drug. Milk contains calcium, which can bind to antibiotics like tetracycline and ciprofloxacin, cutting absorption by 50% or more. For most other meds, milk is fine-but never assume. Always check the label or ask your pharmacist.
Is grapefruit the only fruit I need to avoid?
No. Pomelo, Seville oranges, and some hybrid citrus fruits like tangelos also block the same liver enzyme. If your medication warns against grapefruit, avoid all of them. Regular sweet oranges and lemons are safe.
Why does my doctor say to take my pill before breakfast?
Food slows down stomach emptying and changes acidity, which can block absorption. For drugs like levothyroxine or certain antibiotics, taking them before food ensures your body gets the full dose. Waiting even 30 minutes after eating can cut effectiveness by a third.
Should I take all my pills with food to avoid stomach upset?
No. While NSAIDs like ibuprofen benefit from food, many other drugs-like thyroid meds, antibiotics, and some blood pressure pills-work worse with food. Taking them with food might feel easier on your stomach, but it could make them useless. Always follow the label.
Can I use a pill organizer if I eat at different times?
Yes, but only if you label it clearly. Use sticky notes or a phone alarm to remind yourself: “Take thyroid pill before breakfast,” “Take warfarin after dinner,” etc. A pill organizer helps with timing, but you still need to match each pill to the right meal window. Apps like MyMedSchedule can help personalize this.
What if I forget and take my medicine with food?
Don’t panic. Don’t double up. Just note what happened and take your next dose as scheduled. One mistake won’t ruin your treatment-but if it happens often, talk to your doctor or pharmacist. They can adjust your timing or switch you to a different drug that’s less sensitive to food.
Are herbal supplements safe with my meds?
No more than food is. St. John’s Wort can make antidepressants, birth control, and blood thinners less effective. Garlic and ginkgo can thin your blood like warfarin. Always tell your doctor about every supplement you take-even if you think it’s “natural.”
What to Do Next
Start today. Grab your pill bottles. Look at the label. Write down one thing you didn’t know before. Ask your pharmacist one question. Set a phone reminder for your next dose. That’s it.
You don’t need to be perfect. You just need to be aware. The right timing turns a risky habit into a safe routine. And that’s how you stay in control of your health.

Drew Pearlman
Man, I had no idea grapefruit could turn my statin into a chemical bomb. I’ve been drinking it every morning with my breakfast for years. Guess I’m switching to orange juice now-thank you for the life-saving info. This is why I love Reddit: someone actually tells you the truth instead of selling you a supplement.
RAJAT KD
Take levothyroxine on empty stomach. No exceptions. This is non-negotiable science.
Lindsey Wellmann
Okay but like… I take my blood pressure med with a smoothie and a latte and a croissant and I’m still alive?? 😅 I’m not scared of science, I’m scared of being hungry. Also, who wrote this? I need to hug them. 🤗💊
Micheal Murdoch
This is exactly the kind of practical, no-BS advice people need but never get from doctors who are rushed. I’ve seen patients on warfarin swing from clotting to bleeding because they ate kale salad on Monday and pizza on Tuesday. Consistency isn’t boring-it’s survival. And yes, your pharmacist is your best friend. Don’t be shy. Ask them the dumb questions. They’ve heard them all. I’ve worked in pharmacy for 18 years and I still get new interactions every week. The body’s a complex system, but the rules? They’re simple if you pay attention. Don’t overcomplicate it. Just know your meds, know your meals, and don’t assume anything. Even ‘natural’ doesn’t mean safe. St. John’s Wort isn’t a tea-it’s a drug interaction waiting to happen. And grapefruit? It’s not a fruit. It’s a silent saboteur.
One of my patients, 72, took his simvastatin with grapefruit juice for five years. He ended up in the ER with rhabdo. He didn’t know. Nobody told him. That’s on us. We need to do better. Labels aren’t suggestions. They’re lifelines.
And yes, taking ibuprofen with food isn’t just ‘nice’-it’s preventing ulcers. Your stomach isn’t made of titanium. Treat it like the delicate, sensitive organ it is. Your body doesn’t care if you’re ‘busy’ or ‘forgetful.’ It just reacts. So build habits. Link your pill to brushing your teeth. Set a damn alarm. Use a pillbox. Do whatever it takes. Your future self will thank you.
And for the love of all that’s holy, stop mixing alcohol with meds. Even one drink. You think you’re fine? You’re not. Liver doesn’t care how ‘responsible’ you are. It just metabolizes. And if it’s overloaded? It shuts down. No warnings. No second chances.
This isn’t about diet culture. It’s about basic physiology. Food isn’t the enemy. Ignorance is. And we can fix that-with education, not fear.
Jacob Paterson
Wow. Someone finally wrote this without using the word ‘holistic’ or ‘vibes.’ I’m impressed. Most ‘health’ content is just fearmongering wrapped in kale. But this? This is medicine. Real medicine. Not ‘try this tea for your thyroid.’ Actual science. Kudos. Now if only the FDA would enforce labeling instead of letting pharma bury warnings in 10-point font.
Chris Kauwe
The systemic failure here isn’t patient ignorance-it’s the pharmaceutical-industrial complex’s deliberate obfuscation. CYP3A4 inhibition is not some obscure biochemistry-it’s a well-documented, patent-protected mechanism exploited to sell more pills. Grapefruit isn’t dangerous; the regulatory capture is. They knew. They’ve known for decades. And yet, the labels remain cryptic, the counseling optional, and the liability shifted to the patient. This isn’t a public health issue-it’s a corporate negligence crisis. The FDA’s ‘clearer labels’ are a PR stunt. Real change requires dismantling the profit-driven model of pharmacology. Until then, we’re all just guinea pigs with pill organizers.
Pooja Kumari
I’ve been on warfarin for 7 years. I used to eat a whole bag of spinach every day because I thought ‘more greens = healthier.’ Then I had a stroke. Not a mini. A full one. They told me my INR was 6.8. Six point eight. My blood was basically water. I spent three weeks in the hospital. My husband cried. My cat stopped talking to me. (Okay, maybe the cat was just mad I didn’t feed him.) But after that? I started tracking. Every. Single. Day. Spinach? One cup. Kale? Half a cup. No more random salads. No more cranberry juice ‘for UTIs.’ I use an app now. It’s not glamorous. It’s not Instagram-worthy. But I’m alive. And I don’t take that for granted. If you’re on blood thinners? Please. Please. Just write it down. You don’t have to be perfect. Just consistent. Your life isn’t a diet trend. It’s your only one.
Also, I still eat grapefruit. But only when I’m not on meds. And I check. Always. I’m not brave. I’m just tired of hospitals.
Ian Long
Just wanted to say thank you for this. I’m a nurse, and I see this every day. People think ‘I’ve been taking this for years’ means it’s fine. But the body changes. Your liver slows down. Your diet shifts. Your meds might need adjusting. Don’t be afraid to ask. Don’t be ashamed to say, ‘I don’t know.’ That’s not weakness. That’s wisdom. And if your doctor doesn’t have time to explain? Find a pharmacist. They’re the real heroes here. Also-yes, take your omeprazole before breakfast. I’ve seen people take it after and wonder why their acid reflux is worse. It’s not magic. It’s timing. And timing matters.