Drug Rash Assessment Tool
This tool helps you assess whether your rash might be medication-induced and identifies symptoms requiring immediate medical attention. It is not a substitute for professional medical advice.
Step 1: Rash Characteristics
Step 2: Additional Symptoms
Step 3: Context
Most people don’t think twice about popping a pill - until their skin starts acting up. A red, itchy rash appears out of nowhere. Blisters form. Patches of skin peel. You didn’t change soap, didn’t touch poison ivy, didn’t get sunburned. But you started a new medication last week. That’s not a coincidence. Medication-induced skin reactions are far more common than most realize - and knowing what to look for could save your life.
What Exactly Is a Drug Rash?
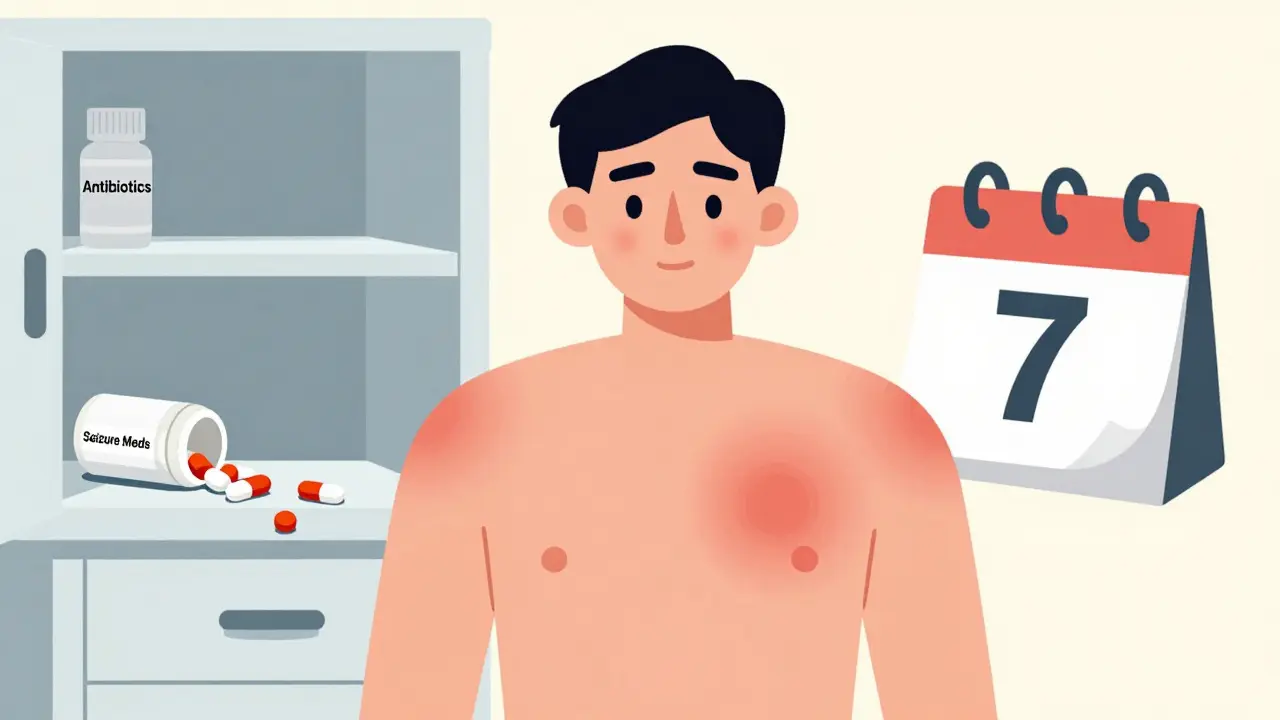
A drug rash is any skin reaction caused by a medication. It’s not always an allergy. Sometimes, it’s just your body reacting badly to a chemical. About 2-5% of all adverse drug reactions involve the skin, according to the US Pharmacist (2022). That means if you’re taking even one prescription or over-the-counter drug, you have a real chance of developing a rash. And it’s not just rare drugs - common ones like antibiotics, painkillers, and seizure meds are frequent culprits.
The most common type is a morbilliform rash - think measles-like spots. It’s red, flat or slightly raised, and shows up symmetrically on your chest, back, or arms. It usually appears 4 to 14 days after starting the drug, but can also show up days after you stop taking it. It’s often itchy, sometimes accompanied by a low fever. The good news? In 90% of cases, it goes away within 1-2 weeks after stopping the medicine. No treatment needed.
When It’s Not Just a Rash - The Dangerous Ones
Not all drug rashes are harmless. Some are medical emergencies. Less than 2% of drug rashes are severe, but they cause 90% of drug-related skin deaths. These are the ones you can’t ignore:
- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN): These start like a flu - fever, sore throat, burning eyes - then your skin begins to blister and peel off in sheets. SJS affects less than 10% of your skin; TEN affects more than 30%. Mortality? 5-15% for SJS, up to 35% for TEN. If you have blisters in your mouth, eyes, or genitals, or if your skin feels like it’s burning and peeling, go to the ER immediately.
- DRESS Syndrome: This isn’t just a rash. It’s a full-body reaction: fever, swollen lymph nodes, liver damage, and high eosinophil counts. It shows up 2-6 weeks after starting the drug. Common triggers? Carbamazepine (35% of cases), phenytoin, lamotrigine, allopurinol, and sulfonamides. It can damage your organs and take weeks to recover, even after stopping the drug.
- Acute Generalized Exanthematous Pustulosis (AGEP): Tiny, non-infectious pustules appear suddenly over large areas of skin. Often triggered by antibiotics like amoxicillin or antifungals. Usually resolves in days after stopping the drug, but needs medical supervision.
These reactions don’t happen to everyone. But if you have certain genes - like HLA-B*1502 (common in Southeast Asians) or HLA-B*5801 (common in Han Chinese) - your risk skyrockets. For example, HLA-B*1502 increases the chance of carbamazepine-induced SJS by 1,000 times. That’s why some doctors now test for these genes before prescribing certain drugs.
What Medications Cause the Most Rashes?
Some drugs are notorious. Here are the top offenders:
- Antibiotics: Penicillins cause 80% of severe allergic drug reactions. Sulfa drugs (like Bactrim) are next. Even amoxicillin - one of the most common prescriptions - triggers rashes in 5-10% of people, especially if they have Epstein-Barr virus (mono) or HIV.
- Antiseizure drugs: Carbamazepine, phenytoin, lamotrigine. These are linked to DRESS and SJS. If you’re on one and get a rash, don’t wait - call your doctor.
- NSAIDs: Ibuprofen, naproxen. These don’t usually cause true allergies, but they can trigger hives or worsen existing skin conditions in 25% of non-allergic cases.
- Allopurinol: Used for gout. Causes 15% of DRESS cases and is the #1 trigger for severe skin reactions in people with HLA-B*5801.
- Diuretics: Hydrochlorothiazide is a major cause of photosensitivity rashes - meaning the rash only shows up where your skin was exposed to sunlight.
- Chemotherapy drugs: Often cause rashes because they attack fast-growing cells - including skin cells.
And here’s a surprise: you might be allergic to a drug you’ve never taken. Trace amounts in food, environmental exposure, or even cross-reactivity can sensitize your immune system. So even if you’ve taken penicillin before without issue, you can still develop an allergy later.

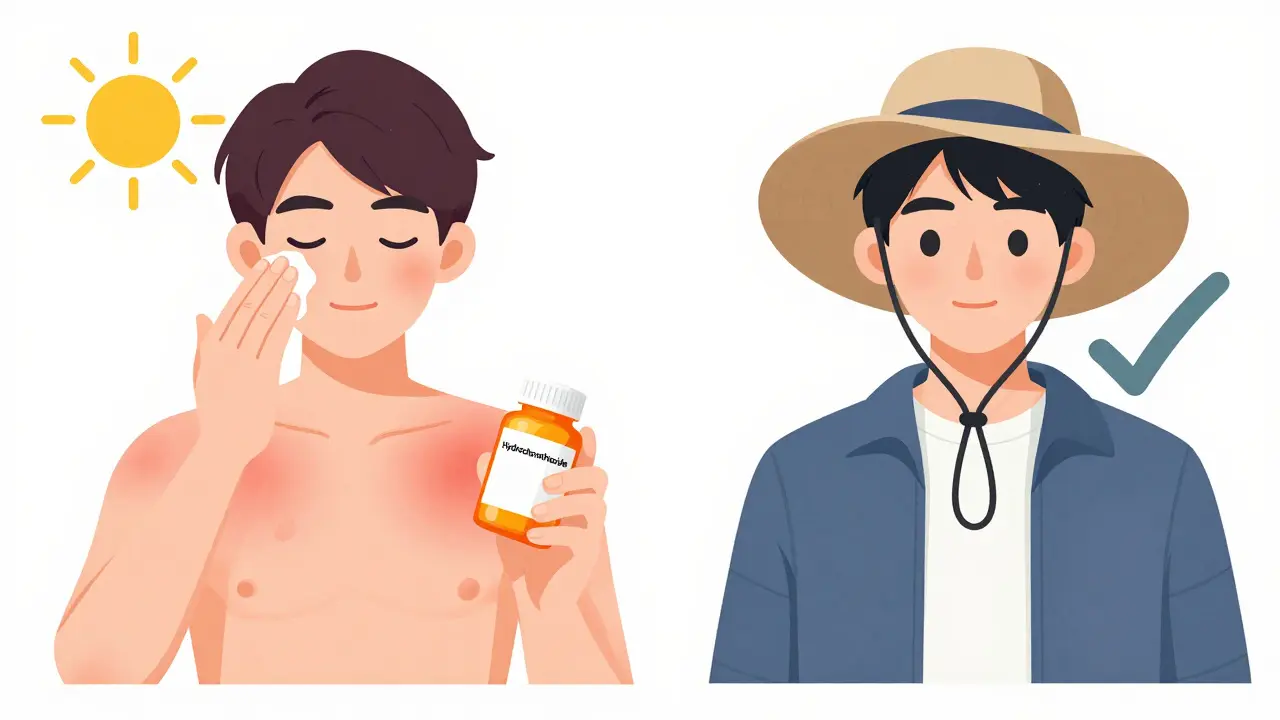
Photosensitivity: The Sun’s Role in Drug Rashes
Eight to ten percent of drug rashes are caused by sunlight. These aren’t sunburns - they’re exaggerated reactions. Your skin turns red, blisters, or peels in areas exposed to UV light, even with sunscreen. Common drugs that cause this:
- Doxycycline
- Ciprofloxacin
- Hydrochlorothiazide
- Amiodarone
- Nonsteroidal anti-inflammatories (like celecoxib)
If you’re on one of these and you get a rash after being outside, it’s likely drug-induced photosensitivity. The fix? Avoid direct sun, wear UPF clothing, and talk to your doctor about switching meds. The rash usually clears within weeks after stopping the drug.
How to Tell It’s a Drug Rash - Not Something Else
Many skin conditions look alike. Eczema, psoriasis, fungal infections - they all cause red, scaly patches. So how do you know it’s the medication?
Look at the timing. If you started a new drug 1-4 weeks ago and the rash appeared soon after, it’s likely related. If the rash shows up symmetrically on your torso and arms, that’s a classic drug rash pattern. If you’ve had the same rash before with a different drug? That’s a red flag.
Drug-induced nummular dermatitis - coin-shaped patches - is often mistaken for eczema. But unlike regular eczema, which can last years, drug-induced cases clear up in 4-8 weeks after stopping the trigger. Doctors miss this in 30-40% of cases, delaying proper treatment.
And don’t assume it’s harmless because it’s not blistering. DRESS can start with mild redness and only show organ damage weeks later. If you feel unusually tired, have yellow eyes, swollen glands, or fever along with the rash - don’t wait.
What to Do If You Get a Rash
Here’s the rule: Never stop a prescribed medication on your own. Stopping an antiseizure drug suddenly can trigger seizures. Stopping blood pressure meds can cause dangerous spikes. Always call your doctor first.
For mild rashes - itchy, red spots, no blisters, no fever:
- Take cool showers. Use fragrance-free, non-soap cleansers.
- Apply over-the-counter 1% hydrocortisone cream twice a day.
- Moisturize within 3 minutes after bathing. Thick ointments like petroleum jelly work best.
- Avoid scratching. Wear cotton gloves at night if needed.
For moderate to severe rashes - blisters, peeling, fever, swelling:
- Stop the drug only if your doctor says so.
- Go to urgent care or the ER.
- Bring a full list of all medications you’re taking - including supplements, vitamins, and herbal products.
- Take a photo of the rash. It helps doctors track changes.
Doctors may prescribe steroid creams (like clobetasol 0.05%) or oral prednisone for severe cases. In DRESS or SJS, hospitalization is often needed. Treatment isn’t just about the skin - it’s about protecting your liver, kidneys, and lungs.
Prevention: How to Stay Safe
The best way to avoid a drug rash? Know your risks.
- Keep a written list of all medications you’ve ever had a reaction to - even if it was years ago.
- Ask your doctor: “Could this drug cause a skin reaction?” Especially if you’re over 65, on 5+ medications, or have HIV, cancer, or autoimmune disease. Your risk jumps to 35% if you take five or more drugs.
- Be cautious with antibiotics if you have mono or HIV. Your rash risk is 5-10 times higher.
- If you’ve been told you’re allergic to penicillin, get tested. About 15% of people who say they’re allergic can actually take it safely. Skin tests now identify 95% of true penicillin allergies.
- Use sunscreen daily if you’re on photosensitizing drugs.
And if you’ve had a severe reaction before, wear a medical alert bracelet. It could save your life in an emergency.
What Happens After the Rash Is Gone?
Once the rash clears, you’re not necessarily done. You may need to avoid that drug forever. Even if you didn’t have a severe reaction the first time, your immune system remembers. Re-exposure can trigger a much worse reaction.
Some people develop long-term sensitivity. Others may have lingering skin changes or scarring. DRESS can cause permanent organ damage if not caught early. That’s why follow-up with a dermatologist or allergist is critical after a serious reaction.
And if you’re on long-term meds - like for epilepsy, gout, or high blood pressure - your doctor may consider alternatives with lower skin reaction risks. For example, if you had a reaction to allopurinol, febuxostat might be a safer option.
Medications save lives. But they can also hurt. The key isn’t avoiding all drugs - it’s knowing the signs, acting fast, and working with your doctor to find the safest path forward.
Can you develop a drug rash even if you’ve taken the medicine before without problems?
Yes. Your immune system can become sensitized over time, even to drugs you’ve taken safely for years. This is why someone might have a severe reaction to penicillin on their fifth course - even if they took it five times before with no issue. Trace exposure, changes in your immune system, or even viral infections can trigger a delayed reaction.
Are drug rashes always allergic reactions?
No. Only about 15-20% of drug rashes are true allergies. Most are non-allergic reactions - meaning your immune system isn’t involved. For example, NSAIDs like ibuprofen can cause hives by directly triggering histamine release. Tetracycline can cause sunburn-like rashes through photosensitivity. These aren’t allergies, but they still require stopping the drug.
How long does it take for a drug rash to go away after stopping the medication?
Mild rashes like morbilliform eruptions usually clear in 1-2 weeks. Drug-induced urticaria (hives) fades within 24-48 hours. Nummular dermatitis takes 4-8 weeks. But severe reactions like DRESS or SJS can take weeks to months to fully resolve, even after stopping the drug. Healing depends on the type of rash and how quickly treatment started.
Can I take a similar drug if I had a rash from one?
It depends. If you had a mild rash from amoxicillin, you might tolerate another penicillin - but not always. If you had SJS from carbamazepine, you should avoid all anticonvulsants in that class. Cross-reactivity is common within drug families. Always consult your doctor or an allergist before trying a similar medication.
Is there a test to confirm a drug allergy?
Yes - but only for a few drugs. Penicillin skin testing is highly accurate and identifies 95% of true allergies. For most other drugs, there’s no reliable test. Diagnosis is based on timing, symptoms, and ruling out other causes. In severe cases, doctors may do a controlled drug challenge in a hospital setting - but only if absolutely necessary and under strict supervision.
Can children get drug rashes too?
Yes. Children are especially prone to rashes from antibiotics like amoxicillin - up to 10% develop a rash, often mistaken for measles. But most are harmless and not true allergies. Still, any rash in a child on a new drug should be checked. If it’s accompanied by fever, swelling, or blistering, seek emergency care.
Should I avoid all medications if I’ve had a drug rash before?
No. Most people who’ve had a drug rash can still take many other medications safely. The key is identifying which drug caused it and avoiding that one - and sometimes its close relatives. Keeping a detailed record and sharing it with every doctor you see is the best way to stay safe without avoiding needed treatments.
veronica guillen giles
Oh wow, another ‘just pop a pill’ guide that somehow forgets to mention the 37 meds my grandma took before her skin peeled off like a bad sunburn. Thanks for the heads-up, doc. Now if only pharma would stop treating our bodies like lab rats with a 5% ‘oops, sorry’ margin.
Also, why is ‘DRESS syndrome’ always the word nobody knows until it’s too late? I swear, if I hear ‘it’s probably just eczema’ one more time…
Ian Ring
Thank you for this incredibly detailed and clinically accurate breakdown. I’ve seen too many patients dismissed as ‘just itchy’ when they were one step from TEN. Please, if you’re reading this and have a new rash + fever + blistering - don’t wait. Call your doctor. Now. Seriously.
And yes, I’ve had patients on amoxicillin with mono who turned into walking red flags. It’s not ‘allergy’ - it’s a system-wide meltdown.
Stay safe. ❤️
erica yabut
How is it still 2024 and we’re still treating human physiology like a software update? ‘Oh, you got a rash? Just stop the drug.’ Like the body isn’t a complex, genetically encoded ecosystem that’s been quietly screaming for decades while Big Pharma cashes in on ‘off-label’ and ‘first-line’ buzzwords.
And let’s not pretend HLA testing is accessible to everyone - unless you’re rich, white, and insured. The real scandal isn’t the rash - it’s the healthcare system that lets you bleed out before it deigns to test you.
Also, ‘photosensitivity’? More like ‘pharma’s silent accomplice.’
Tru Vista
Amoxicillin rash = 5-10% in kids. Not allergy. Just immune overreacting. DRESS = HLA-B*5801. Allopurinol = bad combo. SJS/TEN = ER. Photosens = doxycycline, HCTZ. Stop drug. Don’t scratch. Hydrocortisone. Moisutize. Avoid sun. Done.
Why is this so hard to understand? I’m not even mad. Just tired.
Hank Pannell
It’s fascinating how we’ve outsourced bodily awareness to pharmaceutical labels. We trust a pill to heal us, yet we’re terrified of the signal it sends - a rash - as if the body’s language is noise, not data.
What if the rash isn’t a malfunction… but a message? A biological protest against chemical intrusion? We treat symptoms like bugs to patch, not signals to decode.
Maybe the real epidemic isn’t drug rashes - it’s our refusal to listen to the body until it screams in sheets of peeling skin.
Lori Jackson
Ugh. Another ‘just see your doctor’ cop-out. Have you met the average primary care provider? They can’t even spell ‘DRESS’ without Googling it. And don’t get me started on the 12-hour wait at urgent care while your skin turns into a Jackson Pollock painting.
Meanwhile, the same doctors who prescribe 7 meds to a 72-year-old woman will tell her, ‘It’s probably just dry skin.’
Wake up. This isn’t medicine. It’s roulette with a side of negligence.
Wren Hamley
So let me get this straight - you take a pill, your skin starts acting like it’s been dipped in acid, and the only advice is ‘stop the drug’? What if it’s your blood pressure med? You just gonna go into cardiac arrest to avoid a rash?
And why is it that the drugs that cause the worst rashes are the ones you can’t just quit? Like, I get it - HLA genes are a thing, but why aren’t we screening everyone before prescribing? Why wait for someone to lose 30% of their skin before someone says ‘maybe we should’ve tested?’
It’s not just medical ignorance. It’s economic laziness.
And hey - if you’re on amoxicillin and have mono? Yeah, you’re basically a walking trigger. That’s not ‘bad luck.’ That’s a red flag in a neon sign.
Sarah Little
Just to clarify - you’re saying if I have a rash after taking hydrochlorothiazide, it’s not a sunburn? But I’ve always used sunscreen…
And if I had a rash from penicillin 10 years ago, but never got tested, should I assume I’m still allergic? Or is it possible I’m not?
Also, what if I’m on multiple meds? How do I know which one caused it?
And can I still get the shingles vaccine if I had a DRESS reaction to lamotrigine? I need to know. Please help.
innocent massawe
Thank you for this. In Nigeria, people think rashes are from bad water or evil spirits. No one connects it to medicine. I showed this to my cousin - she was on amoxicillin for a cough, got rash, thought it was ‘heat’ and kept taking it. Now she’s in hospital with fever and swollen face.
May God protect us from ignorance.
🙏
Vincent Sunio
While the article is factually sound, its pedagogical approach is dangerously oversimplified. The conflation of ‘non-allergic reaction’ with ‘harmless’ is a gross misrepresentation of clinical reality. Furthermore, the recommendation to use OTC hydrocortisone for morbilliform eruptions lacks any evidence-based support in dermatological literature - it may mask progression toward more severe phenotypes.
Moreover, the assertion that ‘90% resolve without treatment’ is statistically misleading without context regarding time-to-resolution or patient comorbidities.
Professional responsibility demands more nuance than this.
JUNE OHM
ALLOPURINOL IS A DEEP STATE DRUG. THEY PUT IT IN THE WATER TO MAKE US SICK SO WE’LL BUY MORE MEDS. HLA TESTING? THAT’S JUST A WAY TO TRACK YOUR DNA. THEY WANT TO KNOW WHO’S WEAK. I GOT A RASH AFTER TAKING IBUPROFEN AND THEN MY PHONE GOT HACKED. COINCIDENCE? I THINK NOT. 🇺🇸💣🔥
Philip Leth
Man, I had a rash after taking sulfa back in ‘09. Thought it was just a bad case of heat rash. Took me six months to realize it was the drug. Now I tell everyone - if you’re on anything new and your skin starts acting weird, don’t wait. Call your doc. Don’t Google it. Don’t post on Reddit. Just call.
Also, if you’re from the South? You’re probably allergic to penicillin. Just sayin’.