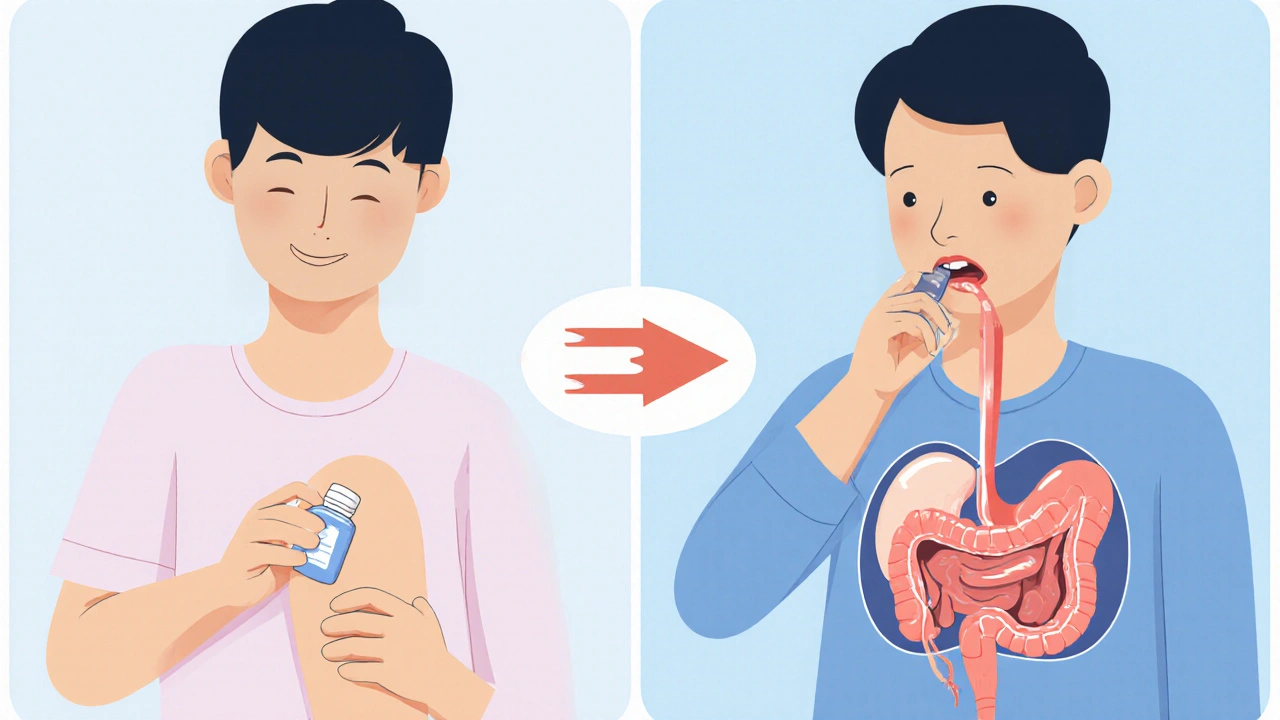
When you have a sore knee or aching shoulder, you might reach for a cream or gel. Or maybe you grab a pill. Both seem to target pain, but they work in very different ways-and the difference matters more than you think.
How Your Body Handles Topical vs. Oral Meds
Topical medications, like gels, creams, or patches, are meant to sit on your skin. They’re designed to work where you apply them: a joint, a muscle, a patch of rash. Oral meds, on the other hand, are swallowed. They travel through your stomach, get absorbed into your bloodstream, and then spread throughout your whole body.
That’s the key difference: systemic absorption. It’s the amount of drug that actually enters your blood. For oral NSAIDs like ibuprofen or naproxen, 70-90% of the dose gets into your bloodstream. That’s efficient-but it also means your liver, kidneys, and stomach are dealing with the full force of the drug.
Topical NSAIDs? Only about 5% or less makes it into your blood. Studies show that even when you apply a full dose of diclofenac gel, your plasma levels stay below 15% of what you’d get from a pill. That’s why doctors now recommend topical NSAIDs as a first choice for localized pain, especially in older adults.
Why Systemic Absorption Matters for Safety
More drug in your blood doesn’t always mean better pain relief. It just means more risk.
Oral NSAIDs are linked to serious side effects. About 15% of people who take them regularly get stomach problems-ulcers, bleeding, acid reflux. The FDA reports 18,432 hospitalizations in 2023 alone from oral NSAID-related GI bleeding. For people over 65, that risk jumps even higher. The American Geriatrics Society says topical NSAIDs cut the chance of GI bleeding by 82% compared to pills.
Topical versions aren’t risk-free. About 10-15% of users get skin irritation-redness, itching, or a rash where the gel was applied. But that’s a far cry from internal bleeding. The FDA’s adverse event database shows just 1.2 reported problems per 10,000 topical NSAID prescriptions versus 14.7 for oral ones.
And here’s something many people don’t realize: topical meds can still enter your bloodstream. If you apply them over a large area-say, both knees, your lower back, and your shoulders-your body can absorb enough to cause effects. One case study found patients using diclofenac gel on 20% of their body surface had blood levels high enough to affect kidney function. That’s why labels warn against using topical NSAIDs on open wounds or under bandages.
When Topical Works-And When It Doesn’t
Topical NSAIDs work well for localized pain: osteoarthritis in the knee, tendonitis in the elbow, muscle strains. Clinical studies show 18-92% of users report good pain relief, depending on the formulation. In a 2023 survey of over 2,400 people with osteoarthritis, 68% said topical gels helped them well. Nearly 90% preferred them over pills-not because they worked better, but because they didn’t wreck their stomach.
But if your pain comes from inside-like a kidney infection, a systemic inflammation, or arthritis affecting multiple joints-topical meds won’t cut it. Only 12% of the 200 most common medications can even be made into topical forms. Why? Most drugs are too big to pass through the skin. Your skin is a tough barrier. It blocks everything from dirt to most drugs.
That’s where oral meds still win. Antibiotics, thyroid meds, blood pressure pills-they need to circulate. You can’t treat a lung infection with a cream. You need the drug to reach every corner of your body.

The Hidden Problems with Topical Use
Even though topical meds are safer, they’re often used wrong.
A 2023 survey of pharmacists found that 41% of topical medication failures happened because patients didn’t use enough. The standard dose? A 4-6 inch ribbon of gel, applied 3-4 times a day. Most people use a pea-sized blob. That’s not enough to reach the joint underneath.
Temperature matters too. Skin absorbs better when it’s warm. If you apply gel in winter, with cold hands and a chilly room, absorption drops. Some users report it takes longer to work when it’s cold-sometimes up to an hour.
And don’t assume “natural” or “OTC” means safe. Many topical products don’t even tell you how much to use. The FDA found only 43% of over-the-counter topical pain relievers give clear dosing instructions. Compare that to 89% of oral meds, which come with exact pill counts and timing.
What About Transdermal Patches?
Don’t confuse topical creams with transdermal patches. They’re not the same.
Topical creams are meant to stay local. Transdermal patches-like fentanyl or nicotine patches-are designed to pump drugs into your blood. They use chemicals to break through your skin barrier. Fentanyl patches can deliver 92% of the drug into your bloodstream, slowly, over 72 hours. That’s why they’re used for chronic pain, not a sore muscle.
But they come with risks too. If you wear a patch and then sit in a hot tub or have a fever, your body absorbs it faster. That’s led to overdoses. Patches are powerful. They’re not for casual use.

Who Should Choose What?
Here’s a simple guide:
- Choose topical if: Your pain is in one spot (knee, wrist, shoulder), you’re over 65, you have a history of stomach ulcers, or you’re on other meds that stress your liver or kidneys.
- Choose oral if: Your pain is widespread (like rheumatoid arthritis), you have deep tissue or internal inflammation, or you need antibiotics, hormones, or other systemic drugs.
And if you’re not sure? Talk to your pharmacist. They can check your meds, your skin condition, and your daily routine to help you pick the safest option.
What’s Changing in 2025
The market is shifting fast. The global topical drug market hit $52.3 billion in 2023 and is growing 7.2% a year-twice as fast as oral meds. Why? Because safety is now a bigger selling point than convenience.
New tech is coming. Microneedle patches, currently in late-stage trials, could deliver drugs like osteoporosis meds through the skin without needles. One study showed 45% bioavailability-close to oral levels-but without the gut damage.
Insurance is catching up. Medicare now covers 82% of topical NSAID prescriptions, up from 67% in 2020. And big pharma is pouring money in. Johnson & Johnson spent $487 million on topical research in 2023. Novartis moved 15% of its NSAID R&D budget to transdermal tech.
By 2030, experts predict 35% of new pain meds will be topical or transdermal. The goal? Cut the 106,000 annual hospitalizations from NSAID-related GI bleeding in the U.S.
Bottom Line: Safer Doesn’t Mean Slower
Topical meds aren’t magic. They won’t fix everything. But for localized pain, they’re the smarter, safer choice for most people. You get relief without the stomach pain, the kidney stress, or the risk of internal bleeding.
Use them right: apply enough, apply often, don’t cover them, and avoid using them on broken skin. And if your pain doesn’t improve in a week? See your doctor. Topical meds are a tool-not a replacement for diagnosis.
The future of pain management isn’t about stronger pills. It’s about smarter delivery. And for millions of people, that means less in your blood-and more relief where you need it.
Can topical NSAIDs cause stomach problems?
Topical NSAIDs rarely cause stomach problems. Less than 1% of users report gastrointestinal issues, compared to 15% with oral NSAIDs. That’s because less than 5% of the drug enters the bloodstream. However, if you apply a large amount over a wide area (like your entire back), enough may be absorbed to cause mild stomach upset. Stick to the recommended dose and avoid covering the area with tight bandages.
Are topical pain relievers as effective as pills?
For localized pain-like a sore knee or elbow-yes, they’re just as effective for most people. Studies show 68-72% of users get good relief with either form. But for widespread pain, deep joint inflammation, or internal conditions, pills are more reliable. Topical meds can’t reach organs or systemic inflammation. They’re great for surface-level pain, not whole-body issues.
Why do some people say topical gels don’t work for them?
The most common reason is under-dosing. Most people use a pea-sized amount, but you need a 4-6 inch ribbon of gel. Other reasons: applying it on cold skin (absorption drops below 32°C), using it too infrequently, or having thick, dry skin that blocks penetration. Some people also have genetic differences in skin absorption-about 18-22% of users simply don’t absorb enough to feel relief, no matter how much they apply.
Can I use topical and oral NSAIDs together?
Generally, no. Combining them increases your total NSAID exposure without adding much extra pain relief. You’re still getting the same active ingredient-just from two sources. That raises your risk of kidney damage, high blood pressure, and stomach bleeding. If one form isn’t working, talk to your doctor about switching, not stacking.
Are transdermal patches the same as topical creams?
No. Topical creams are meant to stay local-only a small amount enters the blood. Transdermal patches are designed to deliver drugs directly into your bloodstream. Fentanyl patches, for example, are powerful opioids meant for chronic pain. They’re not for occasional use. Using a patch like a cream can lead to overdose. Always follow the instructions exactly.
What’s the safest pain reliever for seniors?
For localized pain, topical NSAIDs are the safest choice. The American Geriatrics Society recommends them over oral NSAIDs for people over 65 because they cut the risk of GI bleeding by 82%. Acetaminophen (Tylenol) taken orally is also considered safer than oral NSAIDs, but it’s less effective for inflammation. Always avoid long-term, high-dose use of any pain med-topical or oral-without medical supervision.
Do I need a prescription for topical NSAIDs?
In the U.S., diclofenac gel (Voltaren) is available over-the-counter in a 1% strength. Higher strengths (1.5%) and other NSAIDs like ketoprofen or ibuprofen gel require a prescription. Always check the label. Even OTC topical NSAIDs should be used for no more than 21 days without seeing a doctor. They’re safer than pills, but still medications.
How long does it take for topical pain relief to work?
Most topical NSAIDs start working within 30-60 minutes, but full effect can take 2-4 days of consistent use. Unlike pills, which hit your bloodstream fast, topical gels need time to penetrate the skin and reach the joint. Don’t expect instant relief. Use it 3-4 times a day, even if you don’t feel pain right away. Consistency matters more than speed.
Dalton Adams
Let me break this down for you-topical NSAIDs are basically just placebo with extra steps. 70-90% systemic absorption? That’s the gold standard. If you’re not getting the drug into your bloodstream, you’re not treating anything, you’re just massaging your knee and hoping for the best. And don’t get me started on the ‘it’s safer’ myth-your liver doesn’t care if you rub it on your skin, it still has to process whatever little bit sneaks in. And yes, I’ve read the studies. I’ve read them all.
Charmaine Barcelon
I used Voltaren gel for my knee... and it did NOTHING. I mean, absolutely nothing. I applied it like the instructions said-4 inches, three times a day-and still had to take ibuprofen. So now I’m just like, why bother? It’s a scam. A fancy, expensive scam.
Kane Ren
Honestly? I was skeptical too-but after 3 weeks of using the gel on my elbow tendonitis? I haven’t taken a single pill. No stomach burn, no brain fog, just relief. It’s not magic, but it’s real. And if you’re not using enough? Yeah, it won’t work. But that’s on you, not the medicine.
Karla Morales
The data is clear: topical NSAIDs reduce systemic exposure by over 90%. This isn’t anecdotal-it’s pharmacokinetics. The FDA’s adverse event database confirms a 92% reduction in GI events. What’s being ignored is the bioavailability ceiling: even with optimal application, you can’t achieve therapeutic plasma concentrations for systemic conditions. That’s not a flaw-it’s a feature. But if you’re using it for rheumatoid arthritis? You’re misapplying the tool.
Lisa Detanna
I’m from the Philippines and we’ve been using topical balms for generations-camphor, eucalyptus, menthol. We didn’t need pills for muscle aches. It’s funny how Western medicine keeps rediscovering what other cultures have known forever. The skin is a barrier, yes-but it’s also a gateway. We just need to respect its limits, not force it to be something it’s not.
Jennifer Shannon
I’ve been thinking about this a lot-like, really deeply. The whole idea of ‘systemic absorption’ feels so reductionist, you know? Like we’re reducing pain to a chemical equation. But pain isn’t just biochemistry-it’s emotional, it’s cultural, it’s tied to how we move, how we rest, how we feel seen. Topical meds might not flood the bloodstream, but they force you to slow down-to apply them, to feel the coolness, to touch your body. Maybe that’s the real medicine. The ritual. The mindfulness. The fact that you’re not just swallowing a pill and forgetting about it. I think we’re missing that part in all these studies.
Suzan Wanjiru
If you're using topical NSAIDs, make sure you're washing your hands after. I had a patient who rubbed her knee gel, then touched her eye-ended up with chemical conjunctivitis. Also, avoid heat sources. A heating pad + diclofenac = bad news. And no, you can't use it on your face. Even if you think it'll help your acne. It won't. It'll just make your skin peel.
Henrik Stacke
Fascinating. The shift in pharmaceutical R&D priorities-from volume to precision-is emblematic of a broader healthcare evolution. The American Geriatrics Society’s endorsement is not merely clinical; it is ethical. To prescribe an oral NSAID to an elderly patient without first considering topical alternatives is, in my view, a failure of duty of care. The data is irrefutable. The question is not whether topical NSAIDs are effective-they are-but whether clinicians are sufficiently educated to recommend them. And that, dear colleagues, is the real crisis.
Olanrewaju Jeph
I appreciate the clarity of this post. The dosage issue is critical-most people use a pea-sized amount because they think ‘less is more.’ But the skin isn’t a sponge; it’s a filter. You need the full ribbon. Also, applying it after a warm shower improves absorption by up to 40%. Simple, practical advice that saves people from unnecessary pills. Well done.
Manjistha Roy
In India, we use Ayurvedic oils for joint pain-castor, sesame, turmeric. They don’t enter the bloodstream much either. But they work. Not because of chemistry, but because of consistency. Daily massage. Warmth. Patience. Maybe the real lesson here isn’t about NSAIDs-it’s about slowing down. Taking time. Not rushing to swallow a pill. We’ve lost that. And now we’re paying for it.
Kezia Katherine Lewis
The distinction between topical and transdermal is clinically significant. Topical = local pharmacodynamics. Transdermal = controlled systemic delivery. Confusing the two is like conflating a topical anesthetic with an IV infusion. The pharmacokinetic profiles are fundamentally divergent. Misapplication leads to under-treatment or iatrogenic harm. Clinicians must educate patients accordingly.
Demi-Louise Brown
I’ve been using diclofenac gel for my hip osteoarthritis for six months. No stomach issues. No kidney concerns. Just steady relief. I wish more doctors would start here before prescribing pills. It’s not a second choice-it’s the first.
Ross Ruprecht
Meh. I just take ibuprofen. Works fine.
Bryson Carroll
The whole ‘safer’ narrative is corporate propaganda. Big Pharma knows oral NSAIDs are killing people, so they pushed topical versions as a ‘safer’ alternative to keep people buying. But guess what? They’re still NSAIDs. Still carry the same risks-just slower. And the patch? That’s just a Trojan horse for opioids. Don’t be fooled.
Lisa Lee
I don’t trust American meds. We have real painkillers in Canada-no gel nonsense. Just pills. Strong ones. And if you can’t handle that, maybe you shouldn’t be in pain. This whole topical thing is weak. American weakness.
Laurie Sala
I cried when I realized my mom had been taking 800mg ibuprofen daily for 12 years... and I never knew. She had silent ulcers. I found out when she collapsed. I’m not mad. I’m just... heartbroken. I wish someone had told us about the gel. I wish I’d known. I wish I’d read this sooner. I’m so sorry, Mom.
Javier Rain
This is the kind of info we need more of. Stop letting Big Pharma decide what’s ‘normal.’ You don’t need to swallow a pill for a sore knee. Your body isn’t a chemical reactor. It’s a living system. Treat it like one. Use the gel. Apply enough. Be consistent. And if it doesn’t work after a week? Then go see someone. But don’t just default to the pill. You’ve got options. Use them.