Clot Formation: What It Is and How to Manage It
When working with clot formation, the process where blood changes from a liquid to a gel to stop bleeding, you’re dealing with a double‑edged sword. The same mechanism that plugs a cut can also block a vein or artery if it goes haywire. Understanding the steps behind this transformation helps you spot when it’s protecting you and when it becomes a danger.
One of the most common outcomes of unchecked clot formation is Thrombosis, the medical term for a blood clot that forms inside a blood vessel and may restrict flow. Thrombosis can appear silently in deep veins of the leg – a condition known as deep vein thrombosis (DVT) – or suddenly in arteries, causing heart attacks or strokes. Knowing that clot formation can evolve into thrombosis lets you recognize warning signs early, like swelling, pain, or sudden shortness of breath.
To keep thrombosis in check, doctors often rely on anticoagulant therapy, medications that slow down the clotting cascade and reduce the chance of dangerous clots forming. These drugs, such as warfarin or newer direct oral anticoagulants, work by targeting key proteins in the coagulation pathway. While they’re powerful tools, they require careful monitoring because they can also increase bleeding risk if the dose is too high.
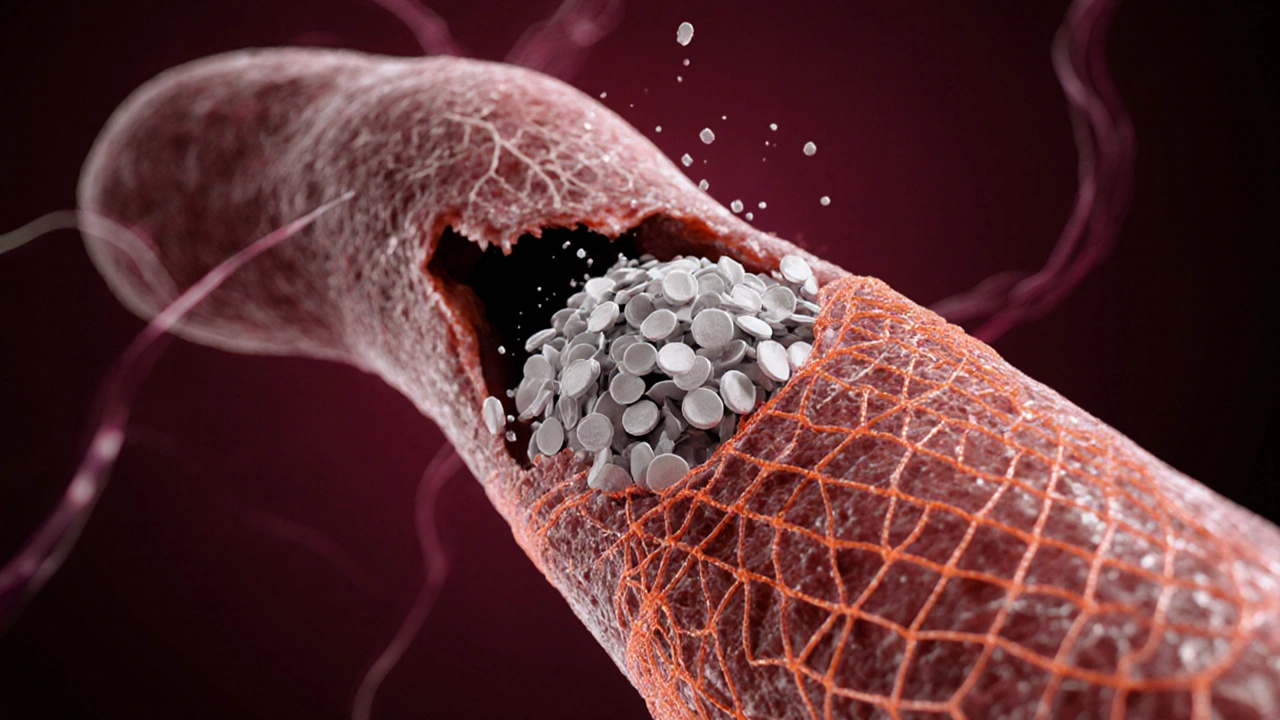
Another critical piece of the puzzle is platelet aggregation, the clumping together of platelets that initiates the early stage of clot formation. When a blood vessel is injured, platelets rush to the site, stick to the vessel wall, and release chemicals that attract more platelets. In healthy people this stops bleeding quickly, but in some cases the aggregation goes beyond what’s needed, laying down a foundation for a larger clot.
Fortunately, your body has its own clean‑up crew: fibrinolysis, the enzymatic process that breaks down fibrin threads and dissolves clots once they’ve served their purpose. Enzymes like plasmin chew through the fibrin mesh, restoring normal blood flow. Certain medical treatments boost fibrinolysis to treat acute clots, but the natural balance between clot formation and fibrinolysis is what keeps circulation smooth.
Why These Players Matter Together
Clot formation, thrombosis, anticoagulant therapy, platelet aggregation, and fibrinolysis form a tightly linked network. The cascade of clotting factors triggers platelet aggregation, which builds a stable clot. If the clot grows too large, thrombosis can block vessels, prompting doctors to prescribe anticoagulants that dampen the cascade. Meanwhile, fibrinolysis works in the background to clear any excess. Understanding this loop helps you see why lifestyle choices, medication adherence, and regular check‑ups are all part of a single strategy.
In the articles below you’ll find practical tips on spotting DVT symptoms, comparing anticoagulant options, and learning how diet and exercise influence platelet behavior. Whether you’re a patient, a caregiver, or just curious about how your blood works, the collection gives you clear, actionable insights that go beyond vague explanations. Dive in to see how each piece fits into the bigger picture of clot health.
How Fibrin Drives Blood Clot Formation
Explore how fibrin transforms a platelet plug into a solid blood clot, its role in the coagulation cascade, related disorders, diagnostics, and treatments.