Coagulation Cascade: How Blood Clots Form and Why It Matters
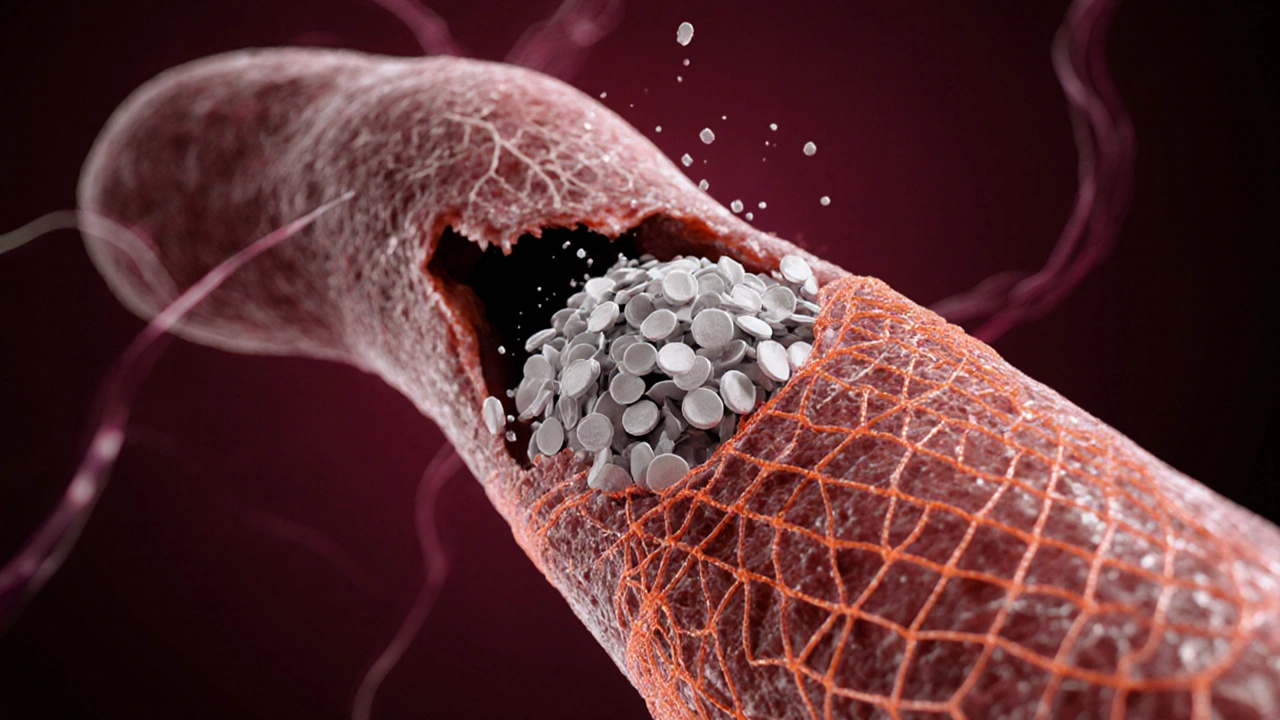
When talking about coagulation cascade, the step‑by‑step series of reactions that turns liquid blood into a solid clot. Also known as blood clotting cascade, it’s the backbone of hemostasis. Right alongside it are clotting factors, a family of proteins that act like dominoes in the process, and fibrin, the thread‑like mesh that actually holds a wound shut. Understanding these pieces helps you see why a problem in any one of them can lead to deep‑vein thrombosis (DVT) or dangerous bleeding.
In simple terms, the coagulation cascade is split into two pathways – intrinsic and extrinsic – that both end at the same finish line: converting prothrombin into thrombin. Thrombin then turns soluble fibrinogen into insoluble fibrin, creating the sturdy net that stops bleeding. Platelets jump in early, forming a plug and releasing chemicals that kick‑start the cascade. Think of it like a relay race where clotting factors hand the baton to the next player until fibrin crosses the finish line. This chain reaction is tightly regulated; too fast, you get clots that block veins, too slow, and you keep bleeding.Why does this matter to everyday health? A disrupted cascade is at the heart of many medical conditions. When clotting goes haywire, you get thrombotic events like DVT, pulmonary embolism, or even stroke. On the flip side, inherited deficiencies (like hemophilia) or medication‑induced drops in clotting factor levels can cause chronic bruising and excessive bleeding. The balance is why doctors prescribe anticoagulants – warfarin, direct oral anticoagulants, or antiplatelet drugs – to dampen specific steps in the cascade and keep dangerous clots at bay.
Key Players in the Coagulation Process
Besides the well‑known factors, vitamin K is a silent partner that helps the liver produce many clotting proteins. Without enough vitamin K, the cascade stalls, which is why warfarin therapy is monitored by checking the INR (international normalized ratio). Another important player is tissue factor, the trigger for the extrinsic pathway that kicks in when blood contacts damaged tissue. Finally, natural inhibitors like antithrombin and protein C act as brakes, preventing the system from overrunning itself. Knowing who does what makes it easier to grasp why certain drugs target specific factors and why lifestyle choices – like staying active or managing stress – influence clot risk.
While the science sounds complex, the practical takeaways are straightforward. If you’ve ever wondered why a leg ache after a long flight might hint at a clot, it’s the cascade in action, forming a clot where blood flow slows. If you’re on an anticoagulant, you’re essentially slowing down one of the steps to keep that clot from growing. And if you have a bleeding disorder, your body’s cascade isn’t completing the final steps, leaving you vulnerable to even minor injuries.
Our collection of articles below dives deeper into each of these angles. You’ll find a guide on how DVT support groups help patients cope with the emotional side of clotting disorders, a clear rundown of different anticoagulant options, and practical tips for managing medications safely. Whether you’re a patient, a caregiver, or just curious about how your body stops bleeding, the posts ahead give real‑world advice backed by the science of the coagulation cascade.
How Fibrin Drives Blood Clot Formation
Explore how fibrin transforms a platelet plug into a solid blood clot, its role in the coagulation cascade, related disorders, diagnostics, and treatments.