Corticosteroids: What They Are, How They Work, and Where They're Used
When your body’s immune system goes into overdrive—attacking your joints, skin, or lungs—it’s often corticosteroids, a class of synthetic hormones that mimic the body’s natural stress-response chemicals. Also known as steroids, they’re not the same as the muscle-building kind you hear about in sports. These are the medicines doctors turn to when inflammation won’t quit, whether it’s from arthritis, asthma, or an autoimmune flare-up.
Corticosteroids work by calming down the immune system and reducing swelling. They don’t cure the root problem, but they buy time—letting damaged tissues heal and symptoms ease. That’s why they show up in so many treatments: for psoriasis, a skin condition where the immune system triggers rapid skin cell growth, they smooth out plaques. For COPD, a lung disease that causes airflow blockage, they help open airways during flare-ups. And in Addison's disease, a rare disorder where the adrenal glands don’t make enough natural steroids, they replace what the body can’t produce at all.
These drugs come in many forms—inhalers for lungs, creams for skin, pills for systemic issues, even injections for severe joint pain. But they’re not harmless. Long-term use can lead to weight gain, bone thinning, or higher blood sugar. That’s why doctors try to use the lowest dose for the shortest time possible. It’s a balancing act: enough to control the disease, but not so much that you risk side effects.
You’ll find corticosteroids mentioned in posts about joint pain, skin conditions, and even dog health—because pets get Addison’s disease too. They’re a tool, not a magic fix. What works for one person might not work for another, and knowing when to use them—and when to avoid them—is key. Below, you’ll see how real patients and doctors use corticosteroids across different conditions, from managing flare-ups to replacing missing hormones. No fluff. Just what works, what doesn’t, and what you need to know before starting or stopping.
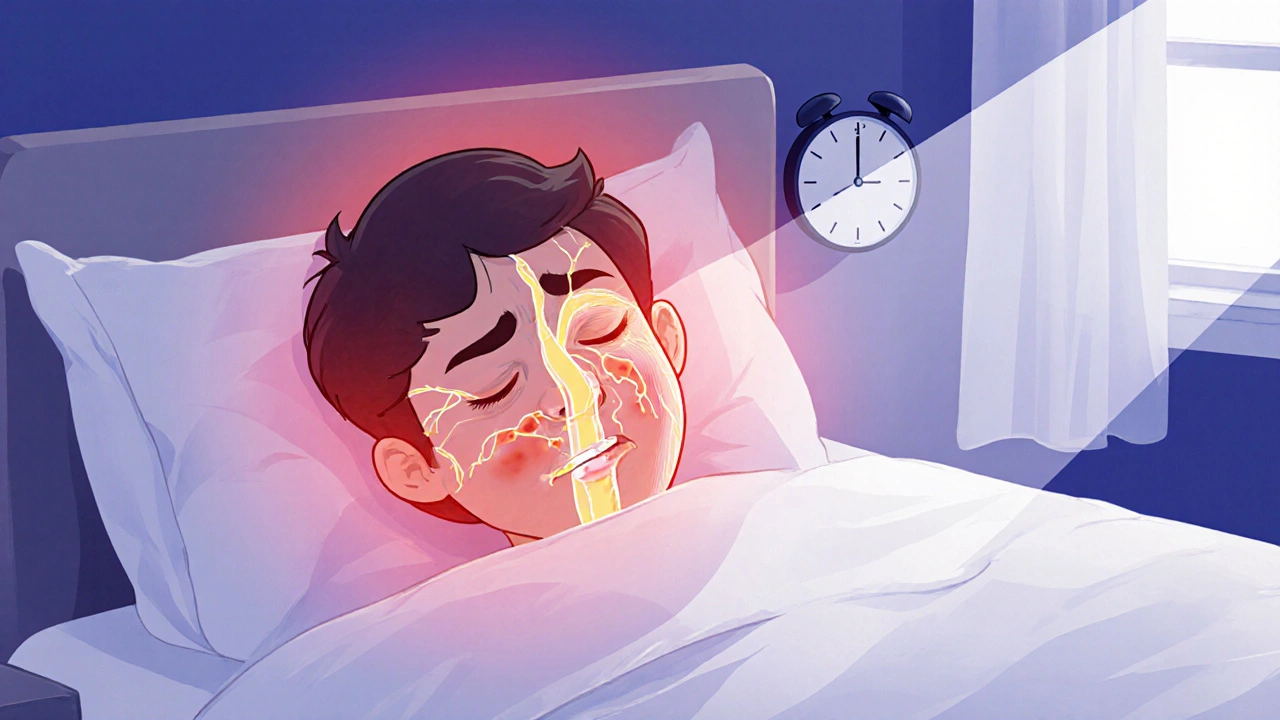
Bell’s Palsy: How Corticosteroids Improve Facial Nerve Recovery
Bell's palsy causes sudden facial paralysis, but prompt corticosteroid treatment can significantly improve recovery. Learn how prednisone works, why timing matters, and what treatments actually help.