Diuretics: What They Are, How They Work, and What You Need to Know
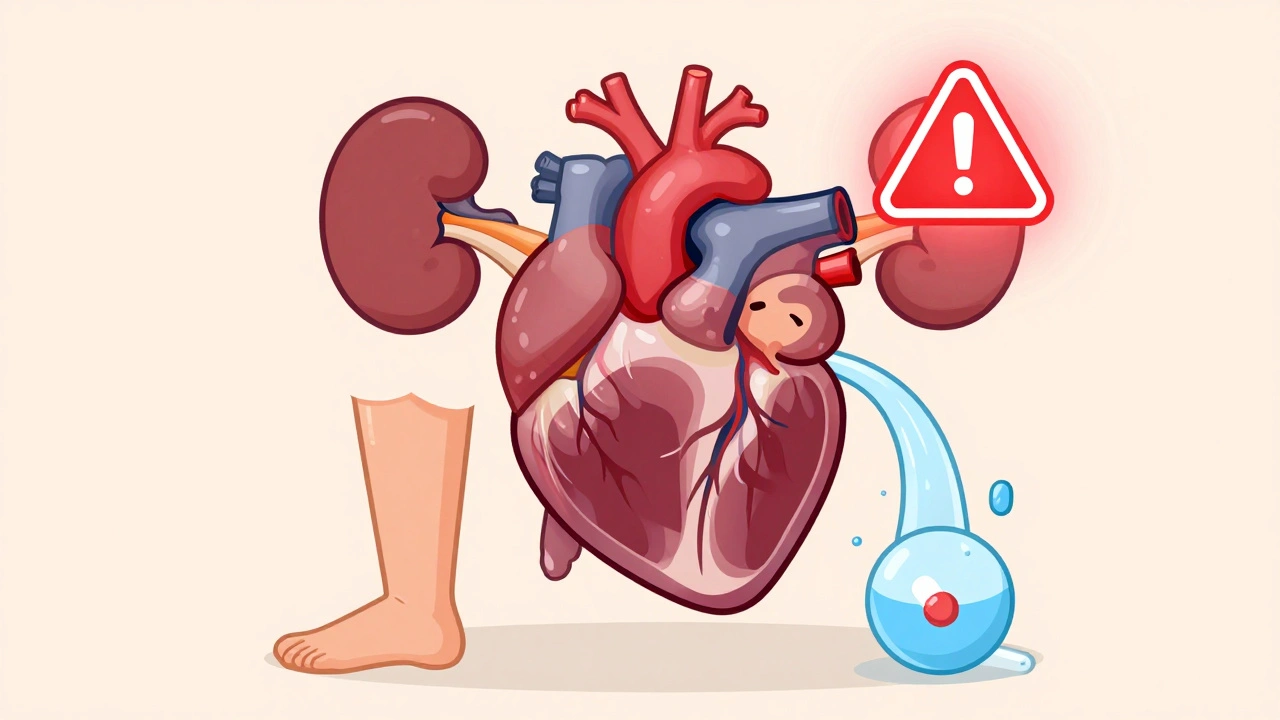
When your body holds onto too much fluid, it can cause swelling, shortness of breath, or high blood pressure. That’s where diuretics, medications that help your kidneys remove extra water and salt from your body. Also known as water pills, they’re one of the most commonly prescribed drug classes in the world. They don’t just make you pee more—they help your heart, kidneys, and blood vessels work better by reducing the strain of too much fluid in your system.
Diuretics come in different types, each with a unique way of acting on your kidneys. Loop diuretics like furosemide work fast and strong, often used for heart failure or severe swelling. Thiazides, like hydrochlorothiazide, are gentler and usually the first choice for high blood pressure. Potassium-sparing diuretics like spironolactone help you keep important minerals while still flushing out fluid. These aren’t interchangeable—each has its own risks and best uses. For example, someone with kidney disease might need a different type than someone with liver swelling. And while many people think diuretics are just for swelling, they’re also a key part of managing heart failure, certain kidney conditions, and even some forms of high blood pressure that don’t respond to other meds.
It’s not just about the drug itself. How you take it matters. Timing can affect your sleep if you take it too late. Salt intake can make them less effective. And mixing them with other meds—like NSAIDs or certain heart drugs—can change how they work or raise your risk of side effects. That’s why knowing what’s in your prescription and why your doctor picked it matters more than you think. Some people worry about losing too much potassium or getting dehydrated, but with the right monitoring, these risks are manageable. The goal isn’t to pee constantly—it’s to find the right balance so your body doesn’t fight against itself.
You’ll find posts here that break down how diuretics fit into real-life treatment plans. Some explain how they’re used with other drugs for heart and kidney conditions. Others cover what to watch for when switching brands or dealing with insurance rules that push for cheaper versions. You’ll also see how they interact with other common meds, what side effects actually happen in practice, and how patients manage them day-to-day. Whether you’re taking one now, considering it, or just trying to understand why your doctor recommended it, this collection gives you the straight facts—not the marketing.
Diuretics and Hypokalemia in Heart Failure Patients: Practical Management Strategies
Diuretics are essential for heart failure but often cause dangerous low potassium levels. Learn practical, evidence-based strategies to prevent and manage hypokalemia safely and effectively.
Hydration and Diuretics: How to Balance Fluid Intake to Avoid Side Effects
Learn how to balance fluid intake while taking diuretics to avoid dehydration, electrolyte imbalances, and dangerous side effects. Practical tips on hydration, electrolytes, and daily monitoring.