Newborn Medication Safety: What Parents Need to Know About Drugs, Dosing, and Risks
When it comes to newborn medication safety, the careful use of drugs in infants under 28 days old to prevent harm from incorrect dosing or inappropriate ingredients. Also known as neonatal pharmacology, it’s not just about giving the right pill—it’s about understanding how a baby’s body processes medicine differently than an adult’s. Newborns have underdeveloped liver and kidney function, slower metabolism, and thinner skin that absorbs topical drugs more easily. A dose that’s safe for a toddler can be deadly for a newborn. That’s why even small errors—like using adult liquid formulas or misreading milligrams instead of micrograms—can lead to serious harm.
Many common medications parents assume are harmless aren’t safe for infants. For example, OTC cough medicine, over-the-counter remedies containing dextromethorphan or phenylephrine are not just ineffective in babies—they’re linked to seizures and breathing problems. The same goes for ibuprofen, a standard pain reliever for older children that can cause kidney damage in newborns. Even something as simple as a topical cream for diaper rash can be risky if it contains corticosteroids or strong antiseptics. What’s surprising is that many of these mistakes happen because parents aren’t told what to avoid—they’re just told what to give.
Pharmacists and pediatricians rely on precise weight-based dosing, not age. A 5-pound baby doesn’t get half the dose of a 10-pound baby—they need a completely different calculation. That’s why pediatric medication errors, mistakes in prescribing, dispensing, or administering drugs to children are among the most common causes of hospital admissions in newborns. Studies show that over 80% of these errors happen because of unclear labels, confusing units (mg vs. mcg), or lack of clear instructions. That’s why tools like easy-open pill caps, child-resistant packaging redesigned for seniors and caregivers with limited dexterity and accessible prescription labels, large-print or braille labels that reduce reading errors matter—even for liquid meds. A misread label can mean the difference between a safe dose and a toxic one.
And it’s not just about what you give—it’s about what you don’t give. Antibiotics are often prescribed for viral infections like colds, but they do nothing for newborns with a runny nose or mild fever. Overuse leads to resistant bacteria, which is especially dangerous in fragile infants. Instead, simple, proven methods like saline drops and suctioning for congestion, or keeping the baby hydrated and monitored, are safer and just as effective. The goal isn’t to treat every symptom—it’s to protect the baby while the body heals naturally.
What you’ll find below are real, practical guides written by pharmacists and pediatric experts. You’ll learn which medications are absolutely off-limits for newborns, how to spot signs of an adverse reaction, why some generics are safer than others, and how to ask the right questions at the pharmacy. No theory. No fluff. Just what you need to keep your baby safe when medicine is involved.
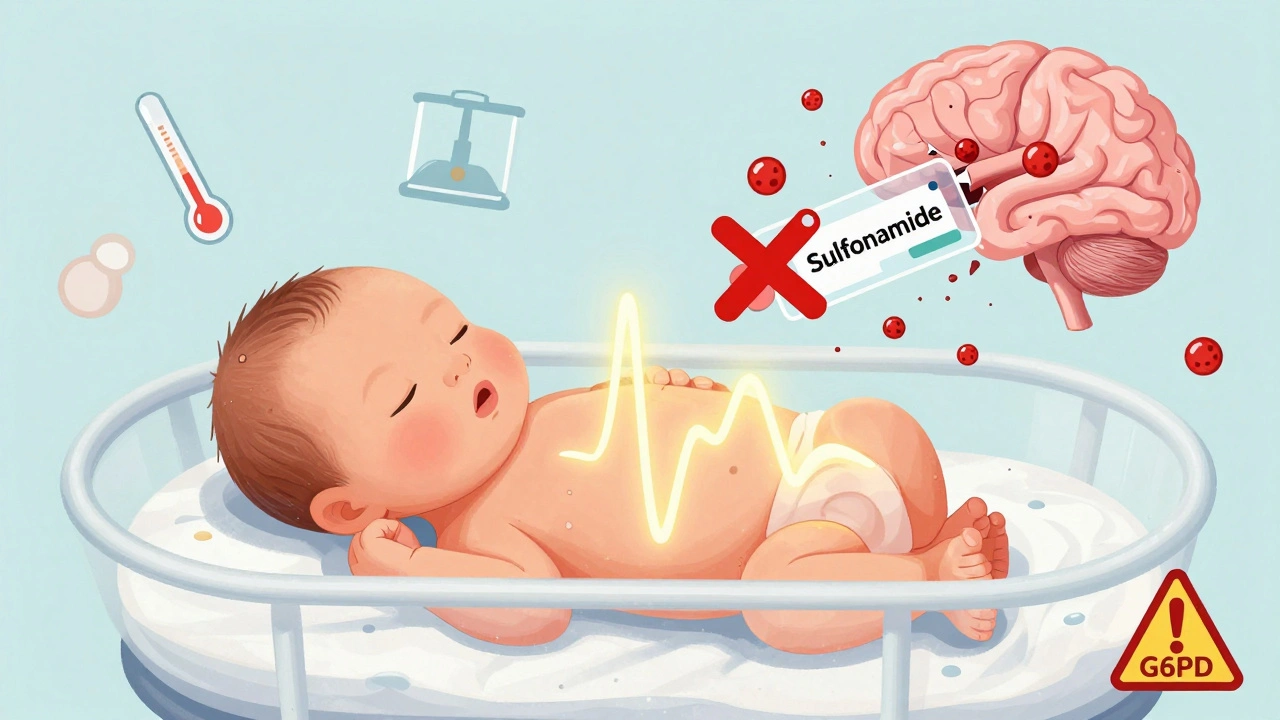
Neonatal Kernicterus Risk: Sulfonamides and Other Medication Warnings
Sulfonamides and other medications can trigger kernicterus in newborns by displacing bilirubin from albumin, leading to brain damage. Learn which drugs to avoid, how risk is assessed, and what parents and providers must do to prevent this preventable condition.