Pharmacy Substitution: What It Is and How It Affects Your Medications
When your pharmacist hands you a pill that looks different from what your doctor prescribed, that’s pharmacy substitution, the practice of replacing a brand-name drug with a chemically identical generic version or another approved alternative. Also known as drug interchange, it’s a routine step in Canadian pharmacies aimed at cutting costs without sacrificing effectiveness. This isn’t a mistake—it’s legal, common, and often encouraged by provincial drug plans. But not all substitutions are created equal, and knowing when it works—and when it doesn’t—can make a real difference in how you feel.
Pharmacy substitution usually involves switching from a brand-name drug like Celebrex to its generic form, celecoxib, or swapping one blood pressure pill for another with the same active ingredient. It’s built into how public drug programs operate: if a cheaper version exists and is approved, they’ll push for it. But this gets tricky when you’re on something like antiepileptic drugs, medications where even small changes in absorption can trigger seizures, or when you’re managing chronic pain with NSAIDs, like ibuprofen or naproxen, where differences in formulation can change how quickly they work. Some people notice a shift in side effects, energy levels, or symptom control after a substitution—even if the active ingredient is the same. That’s because fillers, coatings, and release mechanisms vary between manufacturers, and your body might respond differently.
It’s not just about generics. Sometimes, substitution means trading one drug for another entirely—like switching from gabapentin to pregabalin for nerve pain, or replacing one antidepressant with another that’s covered under your plan. These swaps aren’t always based on your individual needs. They’re often driven by cost, formulary rules, or pharmacy agreements. That’s why it’s important to ask: Is this substitution right for me? If you’ve had bad reactions before, if your condition is unstable, or if you’re on a tightrope of multiple medications, a swap could throw off your whole balance. The posts below cover real cases where substitutions made a difference—sometimes good, sometimes dangerous. You’ll find guides on how to spot when a substitution might be risky, how to talk to your pharmacist about alternatives, and what to watch for after your prescription changes. Whether you’re managing epilepsy, depression, arthritis, or something else, understanding pharmacy substitution gives you control over your treatment—and keeps you safer.
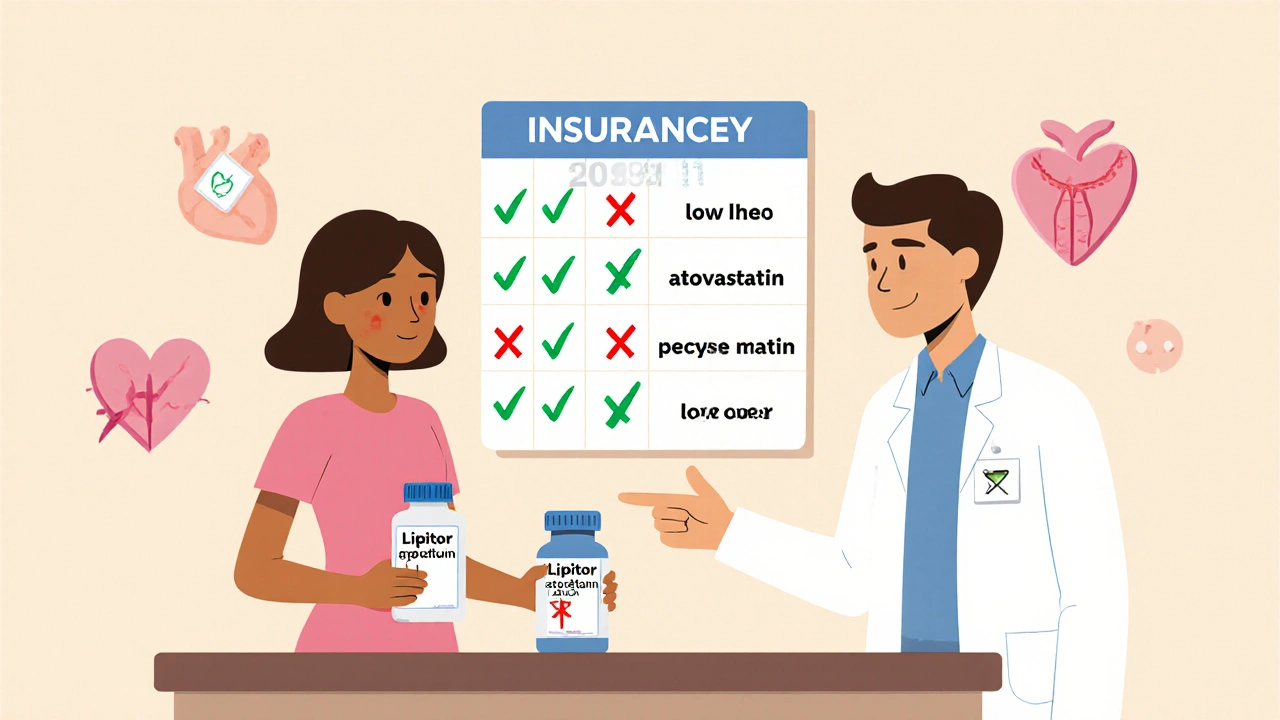
How to Handle Insurance Requirements for Generic Substitution
Learn how insurance companies enforce generic drug substitution, when you can demand the brand-name version, and how to avoid dangerous switches. Real-world rules, state laws, and patient rights explained.