Spirometry: What It Is and How It Helps Diagnose Lung Conditions
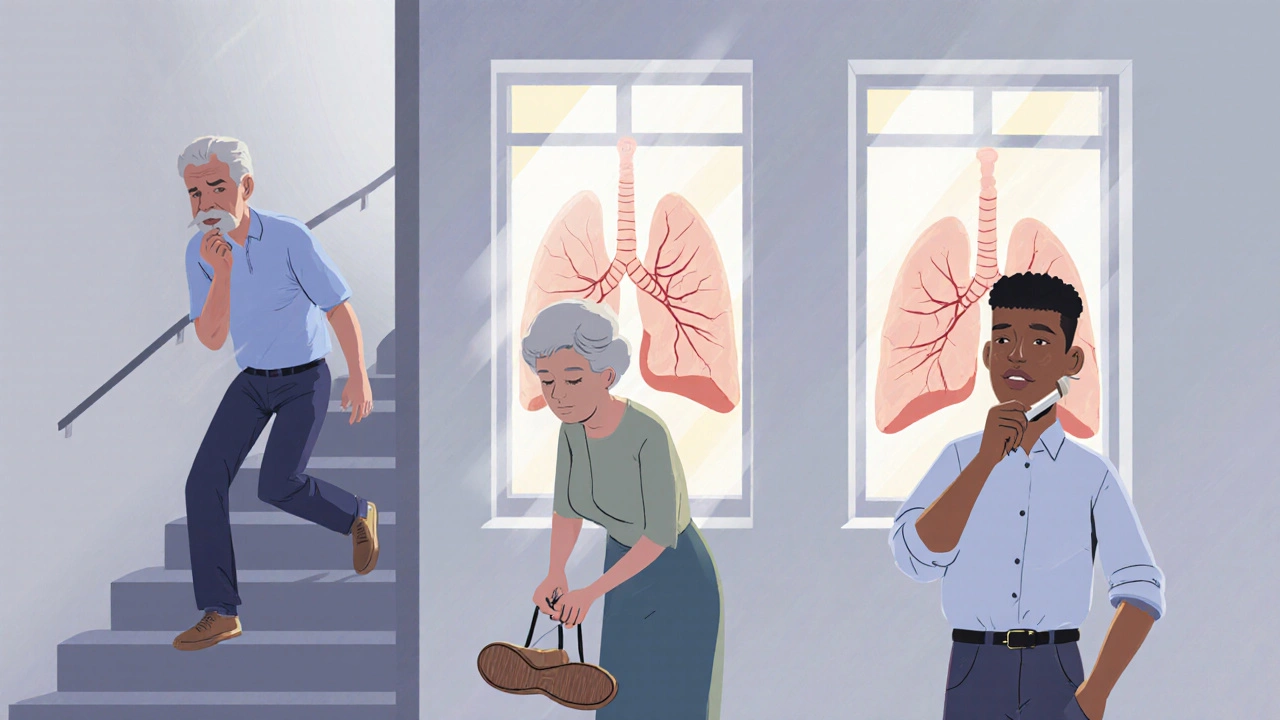
When your doctor suspects a breathing problem, they often turn to spirometry, a quick, non-invasive test that measures how much air you can breathe in and out, and how fast you can do it. Also known as a lung function test, it’s one of the most common tools used to spot problems like asthma, COPD, and other lung diseases before they get serious. Unlike an X-ray or blood test, spirometry doesn’t need needles or radiation—it just asks you to breathe hard into a tube. That’s it. But the data it gives doctors is powerful enough to confirm a diagnosis, track progress, or even rule out conditions that look similar.
This test doesn’t just help people with obvious breathing trouble. Many with early-stage COPD or mild asthma don’t feel symptoms until their lungs are already damaged. Spirometry catches those cases early. It’s also used to check how well treatments like inhalers or pulmonary rehab are working. If you’ve been told you have reduced lung function, this test is the baseline everyone goes back to. It’s not just for smokers or older adults—kids, athletes, and people with allergies can all need it. The results are measured in liters and seconds, giving clear numbers that tell a story: Is your airway narrowed? Are your lungs weak? Can you push air out fast enough?
Related tools like peak flow meters, a simple handheld device that measures how hard you can blow air out, are often used at home by people with asthma to track daily changes. But spirometry is the gold standard in clinics and hospitals. It’s also used alongside other tests like arterial blood gas analysis, which checks oxygen and carbon dioxide levels in your blood—especially when someone’s breathing is severely compromised. These aren’t just lab terms; they’re real tools that help doctors decide if someone needs more medication, oxygen, or even surgery.
You’ll find posts here that dig into how spirometry fits into diagnosing conditions like pulmonary embolism, COPD, and even how it’s used to monitor patients on long-term medications that affect the lungs. Some articles show how breathing tests help adjust treatments for people with chronic illnesses, while others explain why a normal spirometry result doesn’t always mean you’re healthy. Whether you’re a patient trying to understand your test results, a caregiver supporting someone with lung disease, or just curious about how your body works, this collection gives you real, practical insights—not just textbook definitions. The next time you’re asked to take a deep breath and blow hard, you’ll know exactly why it matters.
COPD Explained: Understanding Disease Stages and Effective Treatment Options
COPD is a progressive lung disease with four stages, from mild to very severe. Learn how spirometry measures lung function, what treatments work at each stage, and how to manage symptoms to maintain quality of life.