Systemic Absorption: How Medications Enter Your Bloodstream and Why It Matters
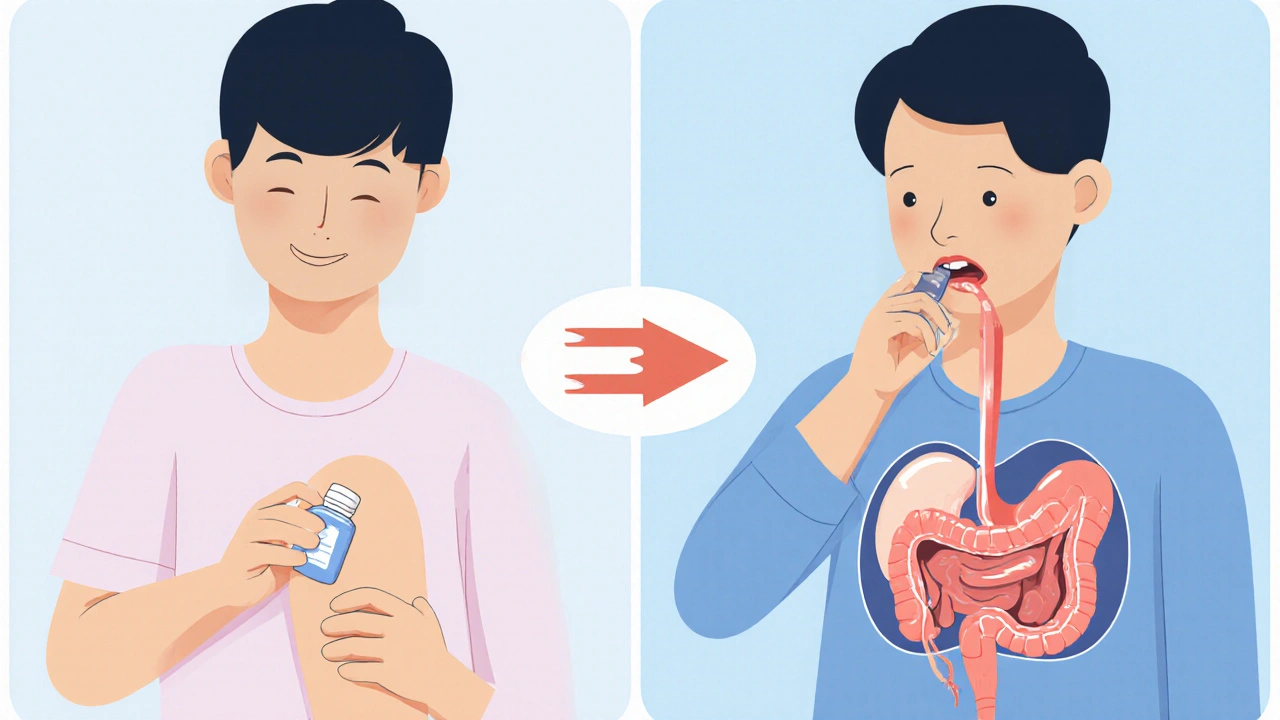
When you take a pill, spray, or injection, systemic absorption, the process by which a drug enters the bloodstream to reach its target throughout the body. Also known as bioavailability, it’s what makes a medicine work—or not. A drug might be powerful on paper, but if it doesn’t get absorbed properly, it’s useless. That’s why two people taking the same dose of the same drug can have totally different results. It’s not about strength—it’s about how your body lets the drug in.
Think about corticosteroids, anti-inflammatory drugs used for conditions like psoriasis, Bell’s palsy, and adrenal insufficiency. When taken orally, they’re absorbed through the gut and spread systemically. But if applied as a cream for skin issues, most of it stays local—unless the skin is broken or the dose is too high. That’s when systemic absorption kicks in, and side effects like weight gain or high blood pressure can show up. Same drug. Different route. Totally different outcome.
It’s the same with proton pump inhibitors, medications like pantoprazole and esomeprazole that reduce stomach acid. They’re designed to be absorbed in the small intestine, not the stomach. If you take them with food, absorption slows down. Take them on an empty stomach, and they work better. That’s not just advice—it’s science. And it’s why some people still have heartburn even though they’re taking their meds.
Systemic absorption also explains why some drugs interact dangerously. Take clopidogrel, an antiplatelet drug used after heart attacks. Some PPIs block the enzyme that activates it. If you take omeprazole with clopidogrel, the PPI reduces systemic absorption of the active form—making the heart drug less effective. That’s not a guess. It’s a documented risk backed by clinical studies.
Even natural supplements like Chirata, a bitter herb used for digestion and blood sugar control rely on absorption. If your gut is inflamed or you take it with a big fatty meal, it might not get into your blood the way it should. That’s why some people say it doesn’t work—they’re not taking it right.
And it’s not just about what you take. It’s about how your body changes. As you age, your stomach acid drops. Your liver slows down. Your gut lining thins. All of that changes how drugs get absorbed. A dose that worked at 30 might not work at 60. That’s why older adults often need different doses—not because they’re weak, but because their bodies process things differently.
Systemic absorption is the invisible link between the pill you swallow and the relief you feel. It’s why some meds work fast, others take days, and some don’t work at all. It’s why your doctor asks if you take meds with food, or if you’ve switched brands. It’s why generic drugs aren’t always interchangeable without checking. And it’s why you can’t just copy someone else’s regimen—even if they have the same condition.
Below, you’ll find real-world examples of how systemic absorption affects treatment outcomes—from psoriasis therapies that need to reach deep tissue, to corticosteroids that can’t be stopped cold turkey, to ED drugs that rely on gut health to kick in. These aren’t theory pages. They’re guides written by people who’ve seen what happens when absorption goes wrong—and how to fix it.
Topical vs. Oral Meds: Which Is Safer and How Much Gets Into Your Blood?
Topical meds deliver pain relief with far less risk than oral pills. Learn how systemic absorption affects safety, effectiveness, and which option is right for your pain.