Generic Substitution: What It Is and How It Saves You Money
When your doctor writes a prescription, you might hear the term generic substitution, the process of replacing a brand-name drug with a chemically identical generic version at the pharmacy. Also known as drug interchange, it’s a legal, safe, and widely used practice that cuts costs without sacrificing effectiveness. Most people don’t realize that the active ingredient in your expensive brand-name pill is exactly the same as the one in the generic version sitting next to it on the shelf. The only differences? The color, shape, packaging, and price—often 80% cheaper.
Generic drugs, medications approved by health regulators as bioequivalent to their brand-name counterparts. Also known as non-brand medications, they must meet the same strict standards for dosage, safety, strength, and how they work in your body. The FDA and Health Canada don’t allow generics to hit the market unless they deliver the same results as the original. That means your generic ibuprofen works just like Advil. Your generic metformin controls blood sugar the same way Glucophage does. And your generic sertraline treats depression just like Zoloft. The only thing changing is the label—and your wallet.
Some people worry that generics are "weaker" or "less reliable." That’s a myth. A 2023 study from the American Medical Association reviewed over 2,000 generic drugs and found no meaningful difference in effectiveness or side effects compared to brand-name versions. The reason brand drugs cost more? Marketing, patents, and profit margins—not quality. Once a patent expires, other manufacturers can produce the same medicine. That’s when drug equivalence, the scientific proof that two drugs perform the same way in the body. Also known as bioequivalence, it’s the backbone of generic substitution. Pharmacists are trained to check this before swapping your prescription. You can ask them to confirm the generic you’re getting is approved and tested.
Not every drug has a generic, but most common ones do: antibiotics, blood pressure pills, antidepressants, cholesterol meds, and pain relievers. If you’re taking a brand-name drug and wondering if a cheaper option exists, just ask your pharmacist. They’ll tell you if a generic is available and if it’s right for you. Some conditions—like epilepsy or thyroid disorders—require extra care with substitutions, but even then, generics are often safe with proper monitoring.
What you’ll find in the posts below are real-world examples of how generic substitution works across different medications—from ciprofloxacin and gabapentin to acyclovir and isotretinoin. You’ll see how people save hundreds a year without losing control of their health. You’ll also learn when to be cautious, how to spot a trustworthy online pharmacy, and why some doctors still hesitate to prescribe generics—even when they should.
Retail vs Hospital Pharmacy: Key Differences in Medication Substitution Practices
Retail and hospital pharmacies handle medication substitution differently: retail focuses on cost and patient notification, while hospitals use clinical teams to optimize drug therapy. Understanding these differences helps prevent errors during care transitions.
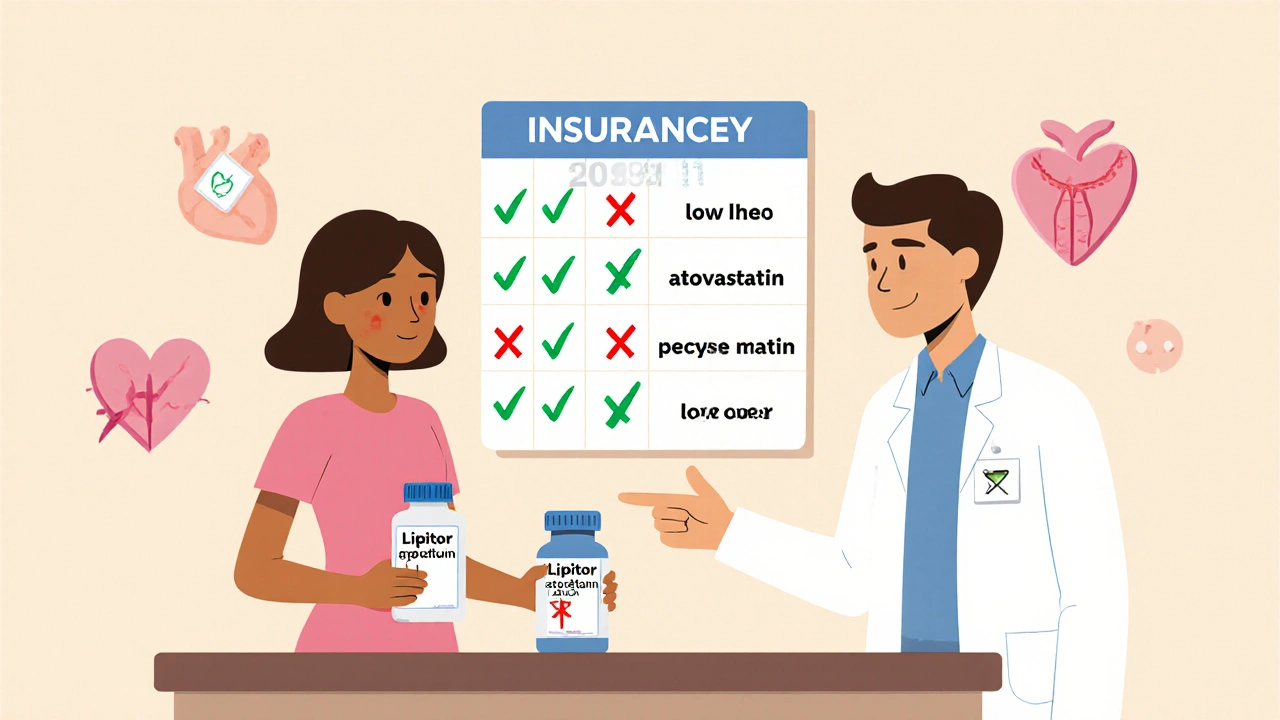
How to Handle Insurance Requirements for Generic Substitution
Learn how insurance companies enforce generic drug substitution, when you can demand the brand-name version, and how to avoid dangerous switches. Real-world rules, state laws, and patient rights explained.